dsm wrote:Snoredog,
You raised the issue in a post 2 days back about the SV calculating Bev's INSP time (BPM=AUTO). I was responding late at night & not able to explore this line fully.
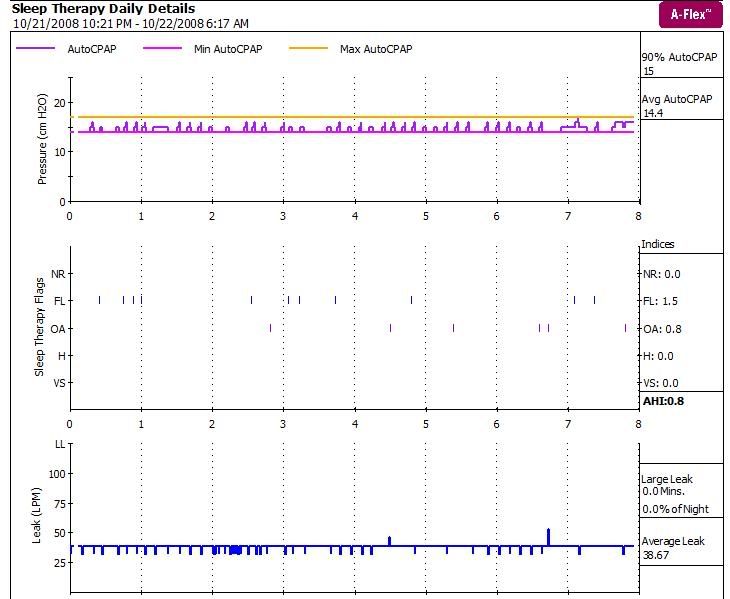
Your point was to do with how the SV might be calculating INSP and the effect this could be having on Bev - IIRC you also said you understood the SV doesn't add PS when in backup mode. We also discussed Bev breathing fast & I pointed out her max BPM didn't exceed 17BPM.
I mentioned I had chosen to do my test using BPM=10 as to evaluate what happens when BPM=AUTO would require me to do it as the live subject & I would need to perfect a way to hold my breath for long periods without inducing leaks or turning blue
Do you want to explore this a bit more as it is an interesting line. If yes can you restate the line of thinking again (am assuming we have even more info that may qualify your thoughts)
DSM
We have a different wave of thinking about this machine. My understanding is Backup Mode or BPM is fixed (when not BPM=Auto), meaning it is just like any other Bipap with a backup mode. When you set BPM=10 for example, it puts that backup mode in fixed mode. So if you set it to BPM=10, you also have to set Inspiration Timer (i.e. Ti) and Rise Time. Now in your video test I think you tired to demonstrate this. Okay, now lets say you set BPM=10, so 60 seconds (1 min/10=6 secs per breath), if a 1.2 sec inspiration time is used that leaves 4.8 seconds for exhale. Now I believe you had set IPAP Max to 25 cm? and EPAP=10?
So on your gage, we should have seen:
EPAP/Minimum pressure =10 cm (we seen that)
IPAP/Min=was at or close to 10 cm (we seen that)
IPAP "working" would move from 10 to 25 cm (we seen that),
but,
if IT timer was 1 second we should have seen it take 1 second for the needle to move up from 10 cm to 25 cm. If it was 2 seconds, 2 seconds, if it was 3 seconds. In other words the higher the IT timer the longer it should have taken to go from 10 to 25.
now,
IF IT timer was shorter, would it stop at the end of the timer before it got to the IPAP Max? Example, if IT was 1.0 would it stop at say 20 cm? We don't know.
If the machine is in fully SV or Auto mode, how does it determine IT time? digital autotrak?
lastly,
If the SV and backup mode is Auto and it uses the "patients" last 4 minutes to determine peak and tidal volumes, does the auto algorithm automatically do the math to lower BPM and set IT and Rise Time? (I'm pretty sure it uses digital autotrack for Rise Time but not sure on the others.
The point to all this is, let's say Bev is breathing really fast maybe 18 BPM and machine finds that and for BPM=AUTO and follows its own protocol of spontaneous BPM -2, that means in backup mode it will set BPM=16, that could still be way too fast for her. I haven't seen a place where you can input the patient's height to know what target volumes should be. Since the range of tidal volume can be from 440ml to 660ml how does it know what is best for Bev?
Your test was very interesting, were you able to observe the LCD and see when the machine was in SV mode vs backup?
Yes, I am still interested in finding out how it finds the ideal IT time.
Note: you can use a
4mm hole to simulate typical mask leak rate so you don't have to turn blue, that is what my manometer has.