Bev, I've been silent on this thread recently because I can't get a grasp of the SV and the reasons for using it.
I'd like to summarize a few points about your condition for all of us - this is all taken from your posts, Please correct the thing I've got
wrong:
You are 5'8", 125 lbs and had been complainning to your doctors for 30 years of an inablilty to sleep.
Your pre cpap AHI was 20 - that was on you sleep study.
viewtopic.php?p=212622#p212622
You got a cpap with Rx fof 16, struggled with it, the doc's response was to drop the pressure to 12 and then to 10.
Your AHI ranged from 28 to 38 on fixed pressure, when you had leak problems
With an Auto at 6-20 you had and AHI of 17.6 and the events came in clusters.
When I was on the straight CPAP I tried lowering my pressure and as it went down the QHIs seemed to go up. At a pressure of
10 it got up to 44. That is whent the Dr. told me that I should be at 19 but he didn't think I could tolerate that pressure so he set it at
16.
You doctor did mention that the next step might be bi-level, and you had a second - bi-level sleep study on which you felt you didn't
sleep at all.
I start out sleeping on my back, but after awhile my back hurts so I turn on my side and then my shoulder hurts, so it's a lot of
tossing and turning and waking up to mask leaks, belching, passing gas, hot flashes. My last sleep study had me waking up 29
times during the night and that was with an Ambien and with CPAP.
I've been 100% compliant for over 8 months and take Melatonin and Ambien every night. I still am wakened numerous times
duting the night with flatuence. As soon as I sit up the air in my stomach comes up, but the air in my gut leaks out all day in the most
uncomfortable and embarassing way!
You never had a follow up for a bi-level, you did insist on an SV in your June 2008 appointment.
A drop to 6.5 to 13.5 raised your AHI and did not help the terrible aerophagia.
You were on Lexapro for most of the first year of therapy, weaned yourself from it sometime in the summer.
viewtopic.php?f=1&t=35018&p=300502#p300502
Another thing that I"ve noticed is that the machine rarely increases pressure when I have an apnea. It doesn't react at all. That's why I have the bottom raised so high. If i let the top pressure go up, I get NRs, so I have to cap that, too. I've been on CPAP for a year and have NEVER woken up feeling refreshed. Although I'm better than a year ago when I was spending 40 minutes a night in apnea.
As I said, I don't understand the SV, and why it was suggested.
For what its worth, this is my summary and interpretation of what I've read:
- You've got sleep apnea - as indicated in your PSG
Your long standing sleep apnea has had a bad impact on your ability to fall asleep and to maintain sleep.
During year on CPAP therapy you've been taking a drug "used to treat mental depression and generalized anxiety disorder" which is also know to inhibit REM sleep, the side effects of which are the following:
More common
Constipation
Decreased interest in sexual intercourse
Diarrhea
Dizziness
Dry mouth
Ejaculation delay
Gas in stomach
Heartburn
Impotence
Inability to have or keep an erection
Increased sweating
Loss in sexual ability desire, drive, or performance
Nausea
Sleepiness or unusual drowsiness
Sleeplessness
Stomach pain
Trouble sleeping
Unable to sleep
(this is from the Mayo clinic). Those are common side effects of that medication, I've colored the one's you've been suffering from.
You are concerned at the lenght of your apneas, and the fact your machine does not raise pressure after they occur.
You are using a machine that needs 3 apneas to happen within a couple of minutes before it figures out it has to raise the pressure.
A I said, I have trouble following the SV discussion -
I would try either a the 420E, which responds to apneas faster than a Respironics and can identify some central apneas and not respond to them (if they occur at all, or a fixed bi-level that would give you the ability to have higher pressure on inhale only.
A PB420E in combinaton with TimeSnapper can let you pin poin exactly what happen before, during and after each apnea, because you can get a
second by second break down of your breathing. (I'll post an example of that breakdown later on).
Once you've really got the Lexapro out of your system - I don't know how long that takes - I would look for a good cognitive behavioral theapist to help you with you sleep problems.
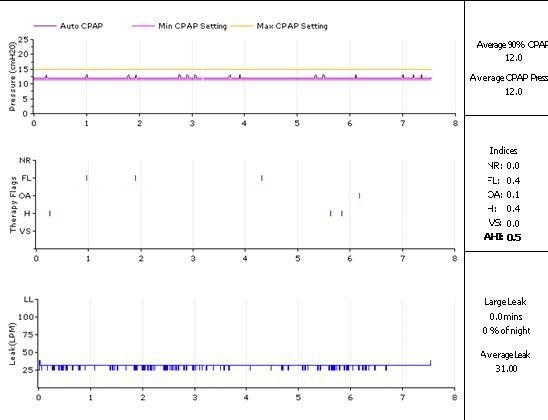
Early on in this thread I suggested the banquet hall on you minimum pressure indicated your breathing pattern confuses the Respironics. Here carboman's recent report, look at the minimum there.
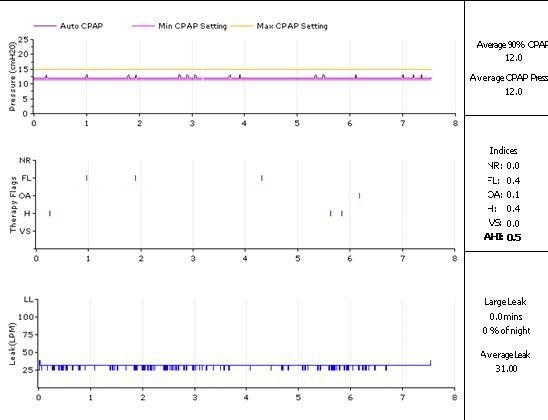
His min. is at his recommended 90%, and his machine is doing very little of that "can we do any better? yes we can , ohno we can't " cycling.
O.