Page 2 of 3
Posted: Thu Feb 28, 2008 8:42 am
by DreamStalker
ZL -
As Den noted, your leaks are probably OK for a full face mask. You may still want to take a look at your nightly charts to see if there is a correlation between your AHI or pressure and the periods of those large leaks.
Your minimum pressure setting seems too low. The machine is not reacting quickly enough to prevent your events because it has to increase the pressure by too much to do so. Setting the min pressure higher allows the machine to get up to the proper pressure more quickly and kill more of those events before they occur. That is why Den suggests setting it at straight CPAP ... but then you have to use a higher pressure for the entire night (even when there are no events to kill ... and that could be cool too if you don't have any side effects like aerophagia).
What pressure to set your minimum at will depend upon what AFLEX setting you have (AFLEX is not an option in CPAP mode, another reason I prefer APAP mode). If your AFLEX is set to 2, you may want to start your min pressure at about 10 or 11 cm and try that for a week or so, then bump it up by 1 cm every week or other week until the AHI stops dropping. You can also try and get yourself a copy of James Skinner's Encore Pro Analyzer ... he is a fellow hose member who developed a very useful tool for Encore Pro users.
Optimizing your treatment requires some patience. The last thing you want to do is start changing your pressure every night or every other night cuz you will just get lost.
I'm sure you will tweak your pressure as quickly as possible ... good luck!
Posted: Thu Feb 28, 2008 2:57 pm
by rested gal
zoolander, I never look at the first three pages of Encore reports. Beginning on page 4 I look only at the
Daily Details graph. I never bother looking at the "Events per Hour" chart.
The Daily Details graph for each night tells me everything I want to know.
If I were using a straight cpap machine at one single pressure, I'd be using 10 or 11.
I choose to use an autopap instead of a straight cpap. In all my autopap tweakings for the past 4 years, I found that I like to set the autopap's MINIMUM pressure at the pressure I'd use if I were using a straight cpap.
Here's what happens if I set an autopap's minimum pressure below the 10 I'd use if I were on straight cpap:
A night with autopap range set for
7 - 20:

Next night with autopap range set for
10 - 20 is much better. That's the range I normally keep my autopap set for, and this is typical of what my data looks like almost every night:

So, since I know that a straight pressure of 10 would probably treat me quite well, why do I use an autopap...using it almost as if it were a straight cpap with my
minimum pressure set at 10?
Here's why:

At three and a half hours into my sleep that night, the machine had to use considerably more than just 10 for me. For a full hour on that particular night the machine was using more than 10...even as much as 13 or 14... to prevent events. I usually sleep on my side, but perhaps I had turned onto my back then AND was in REM.
Either of those (REM or sleeping on one's back) are when apneas usually hit most people hardest, so a scenario in which the two are happening together is a double whammy.
I personally think the minimum pressure is THE pressure to set "right" with an autopap. You can see from those three examples that it doesn't matter (for me, anyway) how high the maximum pressure is set, since the way-up-high pressures aren't ever being used anyway...for me.
What matters is where I set the
minimum pressure in the autopap's range. I set it where it will prevent most events right from the get-go. 10's the magic pressure number for me. Or 11. Or 9. So, min at 10 works great.
Posted: Fri Feb 29, 2008 12:22 pm
by zoolander
I should have posted this here first. I should mention that I suffer from post central apneas at higher pressures
Here's my details and study results
I was recently diagnosed with sever sleep apnea by using a home diagnostic PSG.
I have to be honest and say that even though I have had 2 studies conducted and am currently undergoing a CPAP trial I'm in denial. I haven't got any of the risk factors and generally go to bed at night, fall asleep and wake in the morning feeling as though I have just slept for a good 8 hours. I do wake feeling like I have been hit by a truck. I feel very tired during the day and cannot maintain focus or concentrate. Reading is definiately out of the questions.
Here are my stats:
Age: 36
Height: 181cm
Weight: 78kg
Body Fat %: 10
Blood pressure: 105/60
Resting Heart Rate: 45-50 bpm.
Non Smoker
Non drinker
No medications
Many supplements
Shift worker
I am a young moderately-highly active person. I train in the gym 3 times per week and run 3 times per week. I pretty much exercise everyday. My diet is mainly vegetarian and very healthy. So what the hell is going wrong??
Here are the result of my first study (before CPAP trial) Date: 15/03/2007
Sleep Latency: 4.5 minutes
Sleep Efficiency: 81.9%
Total Arousal Index: 26.9/hr
Respiratory events: SaO2 baseline: Awake=96-98% Asleep = 95-98%
Cyclical in phase hypopnoeas were observed during NREM and REM sleep, in particular in supine REM (Supine REM RDI: 44.5/hr). These events were observed occasionally in association with leg movements, oxygen desaturation and arousal
Average oxygen desaturation: NREM 2%, REM 2%
Oxygen desaturation range: NREM 0-4 %, REM 0-4 %
SaO2 Nadir: NREM 89%, REM 94%
RDI: Total 36.2/hr NREM 35.6/hr, REM 37.6/hr
Periodic Leg Movement: Occasionally associated with arousal and respiratory events
Snoring: mild
ECG: dominant rhythm is sinus with and average of 50bpm. No arrhythmias were present
Conclusion: Severe Sleep Apnea
NOTE: as mentioned I was in denial with these results. I was at the sleep specialist to simply discuss my shift work and they recommended a sleep test and I took it. Initially I thought the test results were just an artifact cause by the bad nights sleep I had with all the equipment attached however the people at the sleep lab told me that the test was technically acceptable and you can obviously see that I go through the various sleep phases (3 supines REM, 4 consolidated SWS with several short wake periods)
Anyhow I just ignored the inital test until I was flicking through an old physiology text book. I'm a PhD student you see and on occasions teach med students. I read that it's quite common for younger people to deal with the sleep apnea because they adapt and have a great physiological reserve. Over time though this changes because the oxygen desaturation and loss of sleep takes toll on the cardiovascular system. Hence I started to reconsider my test results and decides to do a trial on CPAP. Here are the results of my CPAP trail test:
test 2
Here are my stats:
Age: 36
Height: 181cm
Weight: 78kg
Body Fat %: 10
Blood pressure: 105/60
Resting Heart Rate: 45-50 bpm.
Non Smoker
Non drinker
No medications
Many supplements
Shift worker
Here are the result of my first study (before CPAP trial) Date: 05/12/2007
Sleep Latency: 8.5 minutes
Sleep Efficiency: 84.2%
Total Arousal Index: 24.6/hr
CPAP Treatment: SaO2 baseline: Awake=98% Asleep = 94%
CPAP titrated between 4-15cmH2O. Despite CPAP pressure central apneas persisted throughout the study. These were associated with arousal and oxyheamoglobin desaturation. It would appear pressures greater than 10cmH2O are required to control obstructive components, however anything over 12-13cmH2O elicits a significant degree of continuous central events. Response does not seem to be positional or stage dependant. May require review at CPAP clinic to assess for mask/mouth leakage
Average oxygen desaturation: NREM 4%, REM 3%
Oxygen desaturation range: NREM 2-9 %, REM 2-7 %
SaO2 Nadir: NREM 85%, REM 92%
RDI: Total 44.0/hr NREM 43.7/hr, REM 46.3/hr
Periodic Leg Movement: Nil
Snoring: Nil
ECG: dominant rhythm is sinus with and average of 53bpm. No arrhythmias were present
Conclusion: CPAP at 10-11cmH2O appears satisfactory for the control of snoring and obstructive respiratory events. Oxygen saturations are improved on CPAP. Higher pressures are associated with arousals and central events (some post arousal)
NOTE: So at higher pressure I am experiancing central events. This makes sense because I seem to wake at the higher pressures as it seems as though the CPAP at higher pressure is causing me to hyperventilate. Hyperventilation blows of CO2 which lowers [CO2] and hence removes the drive to breath resulting in the central apnea.
I'm really finding it hard to tolerate the CPA and most nights I wake up with the mask off my face. I do remember taking it off but I always try to put it back on but fall alseep. Kind of like when you doze off during the day. You don't quite want to fall asleep but before you know it it's 2 hours later and you can't remember wanting to go to sleep.
I've had all sorts of people giving me advice and I've just been leaving it in the hands of the specialists. My girlfriend does not believe it. For some reason she believes that there is too much room for error with the home sleep tests. I disagree. Some people have said that it could be the shift work and some say that it could be psychosomatic i.e in my head or stress related. I'm a fairly grounded and stable guy so I do not think that's the case.
Anyhow.......any advice would be greatly appreciated. If you know of a similar case please feel free to refer me onto that post.
I look forward to the response(s)
Kind Regards
Zoolander
Posted: Fri Feb 29, 2008 1:19 pm
by ozij
Zoolander wrote:CPAP titrated between 4-15cmH2O. Despite CPAP pressure central apneas persisted throughout the study. These were associated with arousal and oxyheamoglobin desaturation. It would appear pressures greater than 10cmH2O are required to control obstructive components, however anything over 12-13cmH2O elicits a significant degree of continuous central events.
Resmed wrote:Complex sleep apnea (CompSA) is a specific type of sleep apnea where patients exhibit obstructive sleep apnea events, but upon application of positive airway pressure therapy demonstrate persistent central sleep apnea events. This central apnea is most commonly noted while on CPAP therapy, after the obstructive component has been eliminated.
Mayo Clinic Discovers New Type of Sleep Apnea
Friday, September 01, 2006
The complex sleep apnea patients also had fewer complaints about waking up after initially falling asleep than those with central sleep apnea (32 percent vs. 79 percent).
Treatment of complex sleep apnea syndrome: a retrospective comparative review (Sept 2006)...interface problems were more common in CompSAS patients, especially air hunger/dyspnea (0.8 vs. 8.8%) and inadvertent mask removal (2.6 vs. 17.7%) (all P<0.050). CONCLUSION: CompSAS patients have more CPAP interface problems and require more follow-up than OSAS patients but with intervention may have similar treatment results compared to patients with OSAS.
You can disregard the part about effective treatment not having been found, that is no longer true. See the following 2 articles from 2007:
http://www.ncbi.nlm.nih.gov/sites/entre ... xed=google
http://www.chestjournal.org/cgi/content ... 132/6/1839
Here are Resmed, introducing their Adapt SV machine:
http://www.vpapadaptsv.com/PDF/Complex- ... -Sheet.pdf
CompSA is characterized by the following:
• The persistence or emergence of central apneas or hypopneas upon exposure to CPAP or bilevel when obstructive events have disappeared.
• CompSA patients have predominately obstructive or mixed apneas during the diagnostic sleep study, occurring at least 5 times per hour.
• With use of a CPAP or bilevel, they show a pattern of central apneas and hypopneas that meets the Centers for Medicare Services (CMS) definition of CSA (described below).
http://www.vpapadaptsv.com/learn.html - there's a multimedia tutorial.You sound like a typical case -
I think its back to the sleep lab with you, for an ASV (Resmed
or Respironics) titration.
O.
_________________
CPAPopedia Keywords Contained In This Post (Click For Definition):
respironics,
medicare,
Titration,
Arousal,
CPAP,
CSA
Posted: Sat Mar 01, 2008 4:27 am
by zoolander
Ozij,
I had a good look into Complex sleep apnea and spoke to my sleep physican about it. He doesn't believe I have complex sleep apnea. He believes (and showed me with the data gained from my sleep study) that the central apneas are more of a sigh as opposed to an apnea.
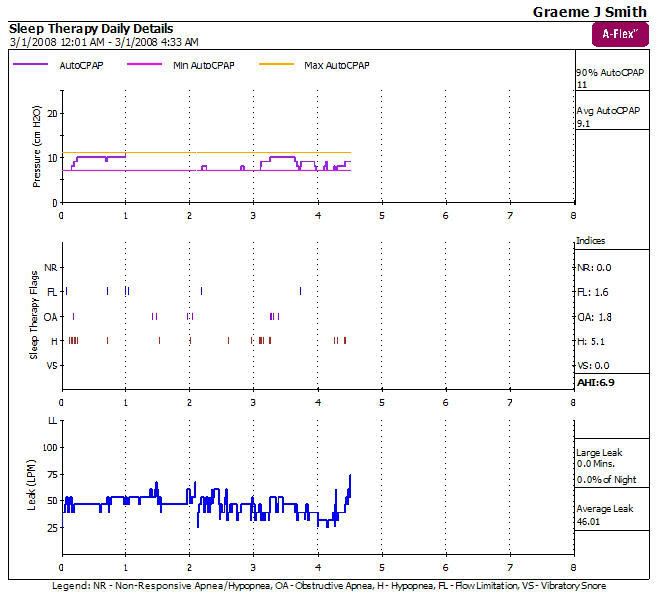
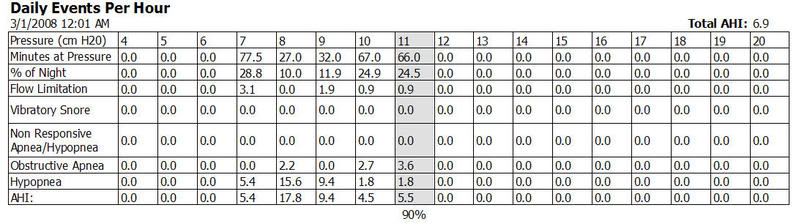
I set my CPAP pressure at 7-11 cmH2O.
Best data so far for me
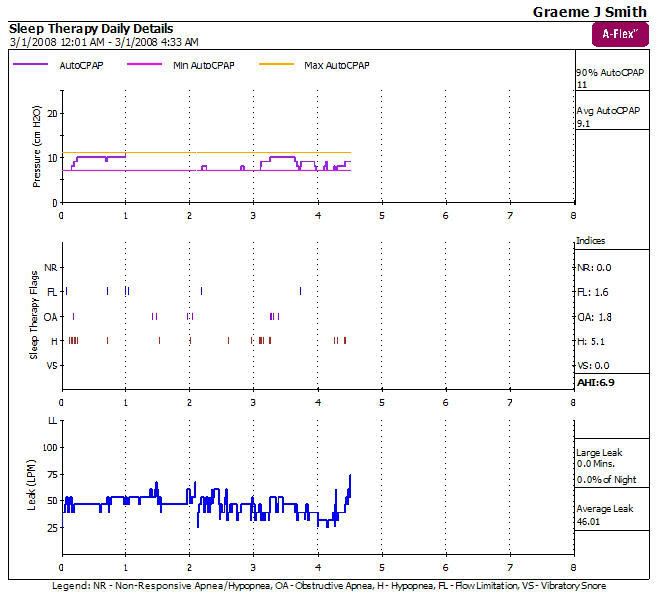
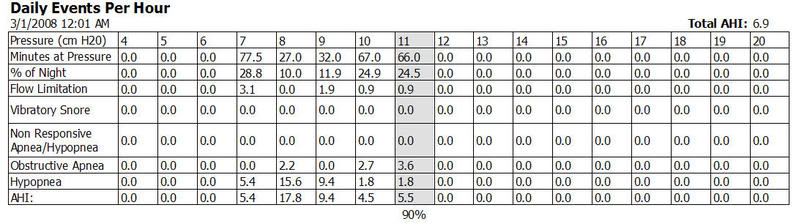
I was pretty shocked by the above data. I sing in a punk rock band and got home from the gig just after midnight. I had to get up for work at 5am. I worked a 10 hour shift and am currently still awake and feeling great at 10pm.
Hence I must have had a good sleep.
I might set the CPAP at 10 to 12 cmH2O. I can see that the lower pressures are to low to stop hypopneas. The Hypopneas dissapear at 10cmH2O and above.
If I get good data tonight using the 10-12 setting I will collect a weeks data and report back
Posted: Sat Mar 01, 2008 7:18 am
by ozij
Well, I'm no doctor.
I wonder how your doctor explained those sighs and their relationship to you desaturatioon ,"
Despite CPAP pressure central apneas persisted throughout the study. These were associated with arousal and oxyheamoglobin desaturation". That sounds to my (admittedly non professional) ears like you were having central apneas with desaturation at all pressures.
Furthermore:
It would appear pressures greater than 10cmH2O are required to control obstructive components, however anything over 12-13cmH2O elicits a significant degree of continuous central events. this too does not sound to me like your obstuctive events were well controlled at any pressure.
I guess the person who wrote this, and the specialist you spoke to interpret the study differently.
As for this comment:
May require review at CPAP clinic to assess for mask/mouth leakage. - it's very apt - your average leak is much higher than your average pressure warrants.
It will be very interesting to see your week's results.
Good luck!
O.
_________________
CPAPopedia Keywords Contained In This Post (Click For Definition):
Arousal,
CPAP
Posted: Sat Mar 01, 2008 12:15 pm
by Goofproof
If you want success you have to get avg leak down below 40 lpm, really under 35 lpm. Jim
Posted: Thu Mar 20, 2008 6:36 pm
by zoolander
It seems as though my baseline leak is at around 40lpm. How and why is this so. When I look at restedgals screenshots her baseline leak is at around the 25lpm mark?
It feels as though my mask fits fine and I check for air leaking out the sides and bottom by placing my hands near the area and in most situations I feel nothing. My mask (Full face Mirage Ultra) does have this are above the nose with holes in it. I've assume that this is to allow the pressure to escape so it doesn't create some sort of vacuum inside the mask. Is that correct? Quite a bit of air comes out of those holes.
Posted: Thu Mar 20, 2008 7:01 pm
by KHENAULT
What mask do you have. Full face masks have a leak rate designed in to clear CO2. You can look up the masks specs for leak rate at a given pressure.
Posted: Thu Mar 20, 2008 9:48 pm
by zoolander
I'm using a Medium Resmed Full Face Mirage Ultra at Pressures 10-12cm H20 AutoCPAP with A-flex.
It looks as though (on the pressure-flow curve) that the mask that I am using allows a vent flow rate of 33-38 cm H20 at pressures 10 and 12 respectively.
Posted: Thu Mar 20, 2008 10:21 pm
by Goofproof
zoolander wrote:I'm using a Medium Resmed Full Face Mirage Ultra at Pressures 10-12cm H20 AutoCPAP with A-flex.
It looks as though (on the pressure-flow curve) that the mask that I am using allows a vent flow rate of 33-38 cm H20 at pressures 10 and 12 respectively.
That shows your leak rate is way out of line, RG uses a different type of mask that has a lower leak rate.
when you get that mask to fit right your leak rate should stay under 40 LPM, 35would be better. Closing you range to 9cm to 12cm will help the numbers but the leaks have to get better. Jim
Posted: Thu Mar 20, 2008 11:30 pm
by rested gal
zoolander, there should be air coming out the exhaust vent area all the time.
Just to be sure that the O2 ports are capped shut though, take a look at the front of your mask. There are two round spots between were the lower strap clips on and the center elbow...two round places that are ports where supplemental oxygen tubes could be attached. Those O2 ports should be covered....with these "Luer lock port caps":
https://www.cpap.com/productpage/port-c ... ies-2.html
Yours are probably capped, as they should be, but just in case.... take a look. There've been a couple of people on the message board that reported one or more caps were missing from their masks when the DME gave them the mask. The people didn't realize air was not supposed to be gushing out those O2 ports.
You really are getting a wayyyy too high leak rate, imho. Perhaps the mask is getting dislodged during the night and you're sleeping through the huge leaks.
Posted: Fri Mar 21, 2008 5:47 am
by zoolander
thanks for your advice guys. yes the caps are sealed.
I'm trying to work out how to dissemble the mask but am afraid that I'm going to break the valve.
I'll run side by side CPAP and pulse ox tonight and post the results
Posted: Fri Mar 21, 2008 8:21 am
by Bert_Mathews
rested gal
I think your examples and definitions were GREAT -- I grabbed them to use at a meeting this weekend..
BETTER than the stuff I had!!
THANKS
BERT
Posted: Fri Mar 21, 2008 8:37 am
by Wulfman
zoolander wrote:thanks for your advice guys. yes the caps are sealed.
I'm trying to work out how to dissemble the mask but am afraid that I'm going to break the valve.
I'll run side by side CPAP and pulse ox tonight and post the results
I would STRONGLY advise NOT taking a UMFF apart. I've seen far too many posts from people who couldn't get them back together correctly and they leaked worse than before......especially in the elbow area.
It doesn't need to be disassembled to be cleaned.
Den