NeoMOAT
Posted: Sat Jan 26, 2008 6:35 am
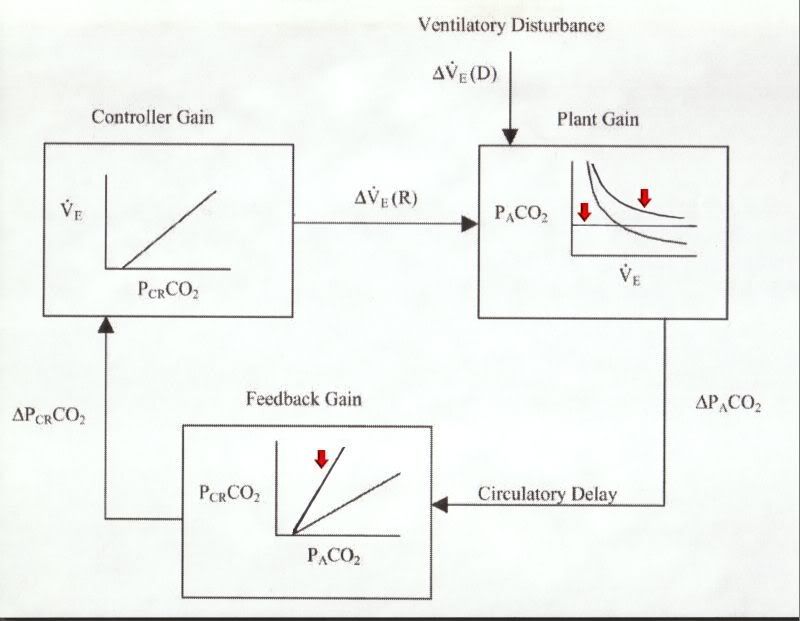
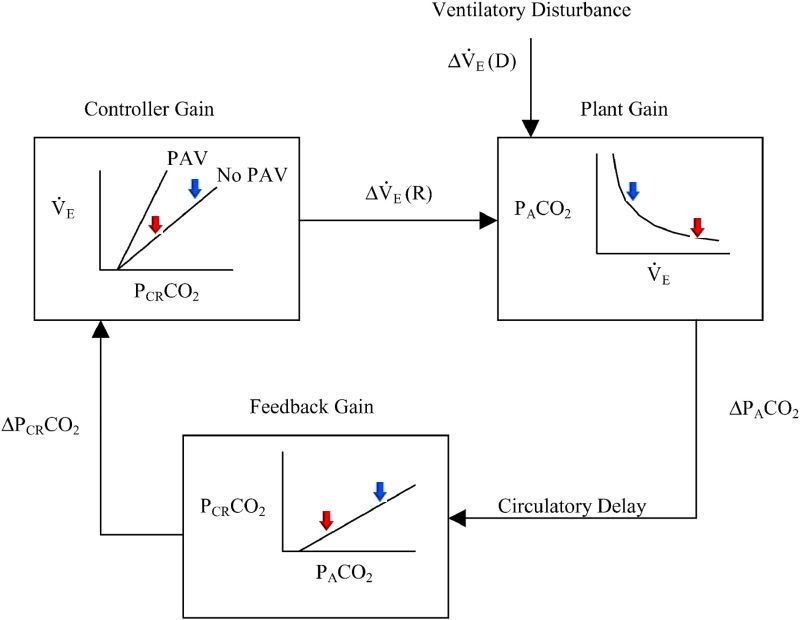
I think one discussion point here that creates a pile of confusion in my mind relates to using the terms "Expiratory Flow Limitation" (EFL) and "Expiratory Intolerance" seemingly interchangeably. I would view these as entirely different entities that would require different tools to quanitify (are they there, and are we using the right data channel to identify them), qualify (do they, in fact, create a problem) and treat (and an equally important concept here is whether treating one entity in one set of criteria results in overall improvement of sleep architecture). Bilevel 25/12 is a bear, and I would also argue that if a patient had a tendency for central apnea you'd be more apt to start that cascade using that modality rather than expecting to see it from "expiratory intolerance". I would also also submit that if central apnea may be/is a concern, I'd be tracking that using some sort of CO2 monitoring device, (on sale this week at Circuit City during their "Red Tag" sale).
Back to the previously submitted waveform:
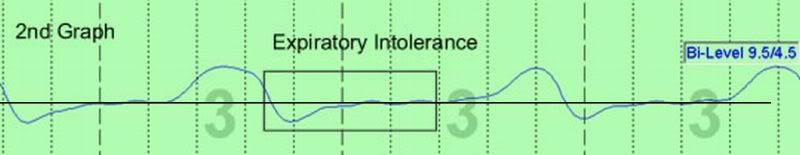
I would question if this is EFL. The first segment is rounded, which is where I would look first for signs of EFL; the phenomenon occurs during periods of zero to near-zero flow, so is it really a flow-anything; the person is now in SWS, which is a more airway-stabilizing sleep state, so it is paradoxical that there is stable airway in light NREM sleep and then it disappears in deep SWS; and in re: exipratory intolerance, if the patient is in SWS, any intolerance would only be exhibited by the sleep technician. And one really needs to look at all the other data channels to properly interpret this. Those "bumps" are occurring at 60 cycles per minute, and if that patient's HR is 60/minute I'd really be thinking "hey, what the heck am I really doing here".
Closer analysis of the other effort channels will greatly assist in the interpretation. In peeling back the onion to micro-analyze waveform, admittedly it's difficult to isolate cause and effect. Not only are there multiple forces contributing to the waveform, but most of them will in turn be affected by another pile of factors (sleep state, anatomy, position, machine, machine mode, acquisition settings).
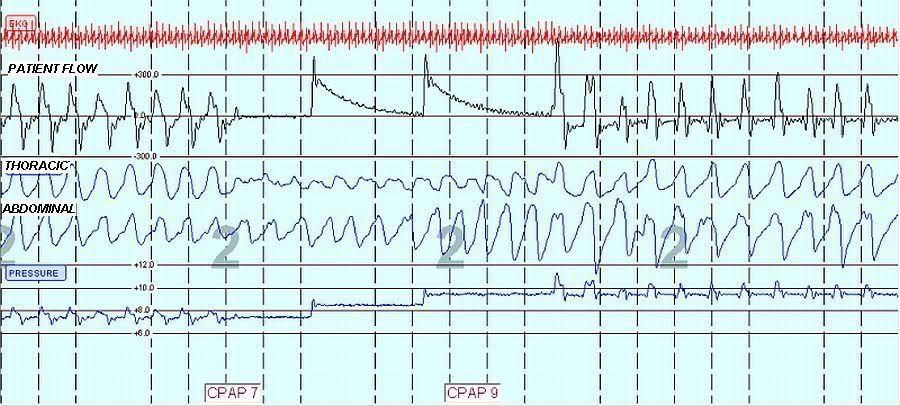
Again, same patient, PB420E, respiratory cycle filtered out of Patient Flow and Abdomen, moving from normal breathing to obstructive apnea (no flow):

The cardiac oscillation has now disappeared from the Patient Flow channel, so this is an opportunity to view the contribution of the machine pressure fluctuations as it reacts to changes in flow and/or patient anatomy. As you can see, they are significant.
SAG
Back to the previously submitted waveform:
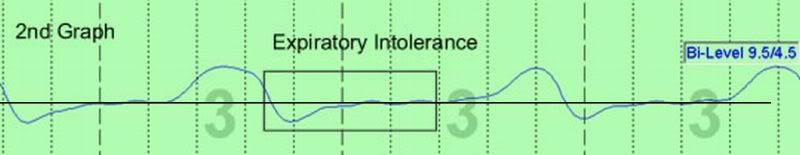
I would question if this is EFL. The first segment is rounded, which is where I would look first for signs of EFL; the phenomenon occurs during periods of zero to near-zero flow, so is it really a flow-anything; the person is now in SWS, which is a more airway-stabilizing sleep state, so it is paradoxical that there is stable airway in light NREM sleep and then it disappears in deep SWS; and in re: exipratory intolerance, if the patient is in SWS, any intolerance would only be exhibited by the sleep technician. And one really needs to look at all the other data channels to properly interpret this. Those "bumps" are occurring at 60 cycles per minute, and if that patient's HR is 60/minute I'd really be thinking "hey, what the heck am I really doing here".
Closer analysis of the other effort channels will greatly assist in the interpretation. In peeling back the onion to micro-analyze waveform, admittedly it's difficult to isolate cause and effect. Not only are there multiple forces contributing to the waveform, but most of them will in turn be affected by another pile of factors (sleep state, anatomy, position, machine, machine mode, acquisition settings).
Again, same patient, PB420E, respiratory cycle filtered out of Patient Flow and Abdomen, moving from normal breathing to obstructive apnea (no flow):

The cardiac oscillation has now disappeared from the Patient Flow channel, so this is an opportunity to view the contribution of the machine pressure fluctuations as it reacts to changes in flow and/or patient anatomy. As you can see, they are significant.
SAG