Page 2 of 5
Posted: Thu Oct 25, 2007 12:04 am
by split_city
mckooi wrote:HI Split_city and SAG,
From the diagrams, what would be the main trigger of the sleep apnea? In sequence, random or cluster?
Mckooi
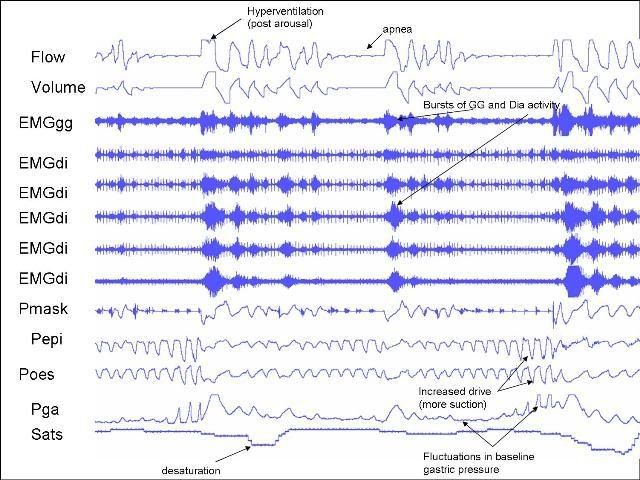
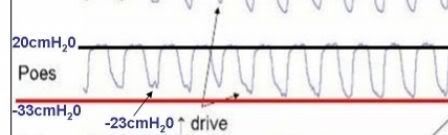
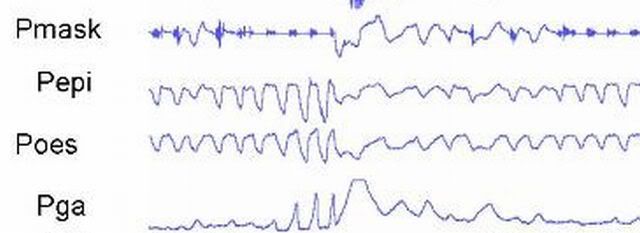
Well, just by the examples I gave you, the loss in tongue muscle tone is likely to be a clear contributor. However, a fall in
lung volume (don't know what the values would be just yet), is also likely to result in airway collapse.
We will also be looking at diaphragm position and the effect of arousal.
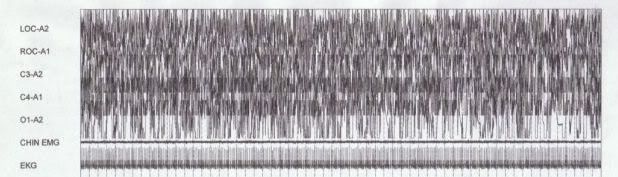
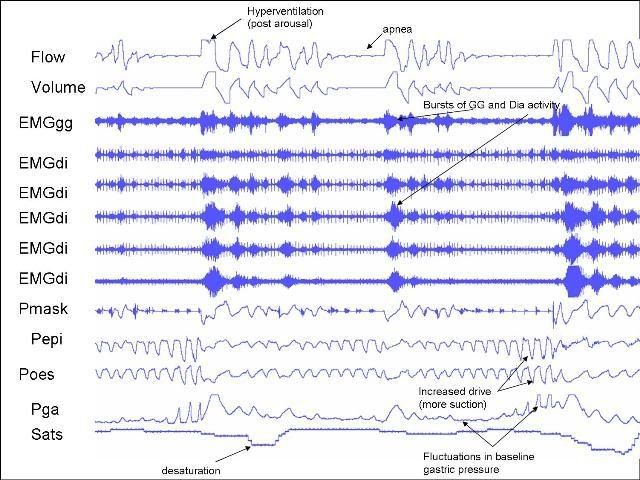
I had the perfect example of a patient last night where his arousals were contributing to his apnea events. This guy had really bad sleep apnea --> AHI over 100 (pretty much all obstructive) with sats dropping into the 60s. I will put a slide up when I'm back at work. Everytime he aroused, he hyperventilated to the point that he blew off his CO2 below his apnea threshold (value at which you switch off breathing). As he went to sleep, had suffered a central apnea. At the same time GG activity was pretty much dead flat. Eventually, CO2 went above this apnea threshold so he bagan to breathe, but his GG was still switched off. Thus, he began to have an obstructive event. He eventually aroused and the cycle began again. It was really freaky watching someone's sats drop so low! He's going in for a CPAP titration study next week so I hope all goes well for him
_________________
CPAPopedia Keywords Contained In This Post (Click For Definition):
Titration,
Arousal,
CPAP,
AHI
Posted: Thu Oct 25, 2007 2:09 am
by Guest
Hi Split_City,
Good findings. Lung capacity and tongue muscle tone were main cause of the sleep apnea. Now, What physical disorder in this case (Obesity (BMI=?), Headache (Morning=Hrs?), Blood Pressure (High=?), Heart Beats (High=Min?), Blood Sugar (High=?), Blood Plasma (Low Oxygen Count=?)...Please lists. I suspect more).
Mckooi
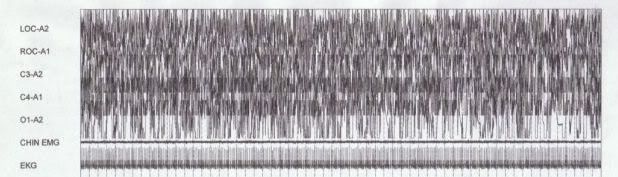
Now, the EEG...
Posted: Thu Oct 25, 2007 4:31 am
by StillAnotherGuest
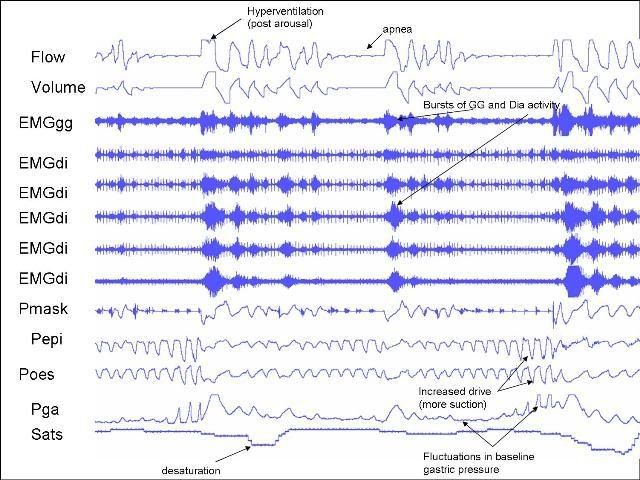
split_city wrote:... there was probably one apnea in the above example.
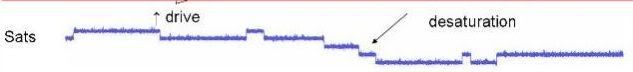
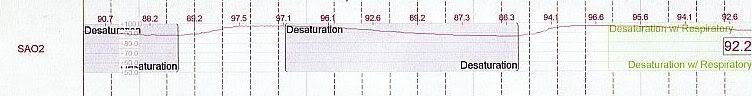
Watchoo mean, Willis? Even if one wanted to be incredibly conservative, that first event would be a hypopnea given the 4% desat. (And if that were the case, then that would make it one of them elusive "central hypopneas" heard tell in the storybooks. But it really should be scored an apnea. The elusive CH remains elusive.)
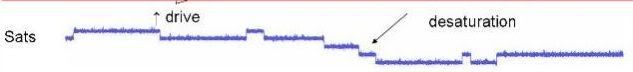
Speaking of which, it would seem that the cause of that staircase effect in the oximetry channel is that your oximeter is only spitting out whole number values when it should be sending tenths (in practical application, it works out to be like 0.4 - 0.5's). Anything screwy in the acquisition values wouldn't seem to create that coincidence (only posting whole numbers).
split_city wrote:Here's another snapshot later in the recording (still SWS)...
Looking forward to taking a look at the simultaneous EEG. Right, continuous SWS with that much respiratory disturbance is quite rare (if not impossible). So don't try to sneak by with C&Ping some 5 year old's
on top of them events. Just cause my boots are covered with Roo Poo don't mean I just blew in from the Outback.
SAG
Posted: Thu Oct 25, 2007 4:53 am
by dsm
Hi SplitCity
Thanks for starting a really informative & interesting thread a feeding frenzy for us OSA folk who have partially recovered - starved of good intellectual OSA stuff (proof being, look at the folk you have harvested)
Your charts are very informative & thanks for the commentary (& the other posters questions).
DSM
Really appreciative !
The Infamous "One More Thing"...
Posted: Thu Oct 25, 2007 5:10 am
by StillAnotherGuest
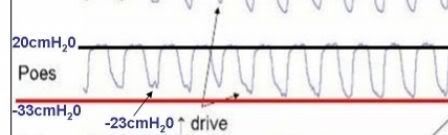
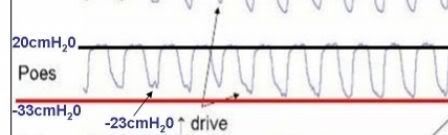
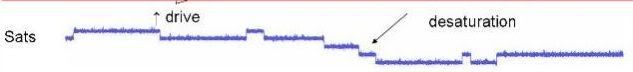
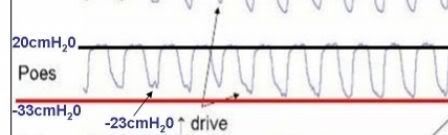
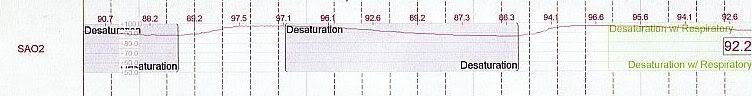
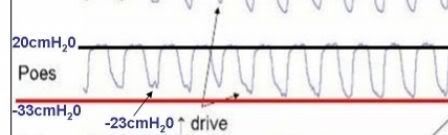
A 53 cmH2O swing during "normal" breathing?
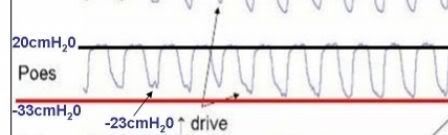
Just how beefy is this guy?
SAG
Posted: Thu Oct 25, 2007 6:25 am
by split_city
StillAnotherGuest wrote: split_city wrote:... there was probably one apnea in the above example.
Watchoo mean, Willis? Even if one wanted to be incredibly conservative, that first event would be a hypopnea given the 4% desat. (And if that were the case, then that would make it one of them elusive "central hypopneas" heard tell in the storybooks. But it really should be scored an apnea. The elusive CH remains elusive.)
Are you referring to this snapshot??

I would have assumed the first event was an apnea due to the cessation in flow. The others would be hypopneas? I'm not a polysomnographer so my understanding of the scoring criteria is a bit rusty
StillAnotherGuest wrote:Speaking of which, it would seem that the cause of that staircase effect in the oximetry channel is that your oximeter is only spitting out whole number values when it should be sending tenths (in practical application, it works out to be like 0.4 - 0.5's). Anything screwy in the acquisition values wouldn't seem to create that coincidence (only posting whole numbers).
The readings on the oximeter we have (in our research room anyway), only displays whole numbers. The actual data in our acquisition displays values up to two decimal places.
StillAnotherGuest wrote:split_city wrote:Here's another snapshot later in the recording (still SWS)...
Looking forward to taking a look at the simultaneous EEG. Right, continuous SWS with that much respiratory disturbance is quite rare (if not impossible). So don't try to sneak by with C&Ping some 5 year old's
Well, I'm not going to argue with you on that . There probably were arousals during his SWS period but I probably missed them as I have to watch 3 computers at once.
It definately will be interesting to find our how many events were associated with arousals. It will help us to try and decipher why there are generally less events and less severe events during SWS. Perhaps this increased arousal threshold during SWS isn't fiction?
SAG
Re: The Infamous "One More Thing"...
Posted: Thu Oct 25, 2007 6:29 am
by split_city
StillAnotherGuest wrote:A 53 cmH2O swing during "normal" breathing?
Just how beefy is this guy?
SAG
Yep, those values are correct. I wouldn't call it "normal" breathing as he was quite flow limited. His airway was acting like a Starling resistor. Drive was very much increased!
All my subjects are obese. His BMI was around 32
Posted: Thu Oct 25, 2007 6:40 am
by split_city
I have a question for you:
Just say the below "event" lasted >10secs and sats dropped by >3%, would it be called a hypopnea or apnea? This has happened in a couple of my patients in that there was no inspiratory flow but very small expiratory flow. I can confirm no inspiratory flow as I was in the room watching and listening to the patient during some of these types of events. I could only hear a small "expiratory" snore.

_________________
CPAPopedia Keywords Contained In This Post (Click For Definition):
Hypopnea
_________________
CPAPopedia Keywords Contained In This Post (Click For Definition):
Hypopnea
_________________
CPAPopedia Keywords Contained In This Post (Click For Definition):
Hypopnea
Posted: Thu Oct 25, 2007 6:46 am
by split_city
dsm wrote:Hi SplitCity
Thanks for starting a really informative & interesting thread a feeding frenzy for us OSA folk who have partially recovered - starved of good intellectual OSA stuff (proof being, look at the folk you have harvested)
Your charts are very informative & thanks for the commentary (& the other posters questions).
DSM
Really appreciative !
No worries. I thought it would be nice to let you OSA folks out there know what type of research is being conducted in regards to the pathophysiology of OSA.
Posted: Thu Oct 25, 2007 6:18 pm
by RosemaryB
Do you know what, if any, role a hiatal hernia might play in OSA? Seems like there might be a connection.
On Various...
Posted: Thu Oct 25, 2007 7:29 pm
by StillAnotherGuest
split_city wrote:Are you referring to this snapshot??
No, this one:

split_city wrote:The readings on the oximeter we have (in our research room anyway), only displays whole numbers. The actual data in our acquisition displays values up to two decimal places.
Yeah but the graph is only reporting out whole numbers so it ends up choppy like
instead of smooth like
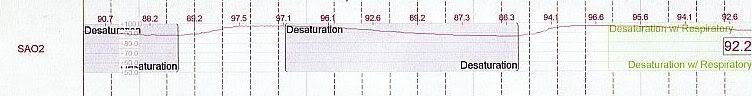
Further, the numbers are getting rounded off, so you're missing up to 0.4s here and there.
split_city wrote:I have a question for you:
Just say the below "event" lasted >10secs and sats dropped by >3%, would it be called a hypopnea or apnea?
An apnea. The new rules say >90% reduction in thermal flow, without regard to any desaturations. However, use of 3% as a desat is an accepted alternative definition for hypopneas (4% is recommended).
split_city wrote:StillAnotherGuest wrote:A 53 cmH2O swing during "normal" breathing?
Just how beefy is this guy?
SAG
Yep, those values are correct. I wouldn't call it "normal" breathing as he was quite flow limited. His airway was acting like a Starling resistor. Drive was very much increased!
All my subjects are obese. His BMI was around 32
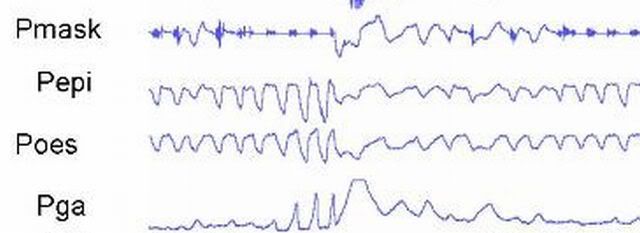
A question I have then regarding the "swing" is not the 33 cmH2O nadir but the 20 cmH2O positive inflection. Exhalation is passive, even in OSA, so baseline
Pes is normally 0 cmH2O. I imagine with massive forces on the airway, you could require large positive pressures for exhalation, but that wouldn't be obstructive apnea, that would be obstructed airway requiring tracheostomy. Asthma might show high
Pes on exhalation, but the expiratory limbs of the waveform are not prolonged. Or, are you doing the compressed abdomen thing.
RosemaryB wrote:Do you know what, if any, role a hiatal hernia might play in OSA? Seems like there might be a connection.
I got nothing on that one.
SAG
Re: On Various...
Posted: Thu Oct 25, 2007 8:00 pm
by split_city
StillAnotherGuest wrote: split_city wrote:Are you referring to this snapshot??
No, this one:

Well that's where the confusion lies as I was referring to the other snapshot when talking about the apnea .
StillAnotherGuest wrote: split_city wrote:The readings on the oximeter we have (in our research room anyway), only displays whole numbers. The actual data in our acquisition displays values up to two decimal places.
Yeah but the graph is only reporting out whole numbers so it ends up choppy like
instead of smooth like
Further, the numbers are getting rounded off, so you're missing up to 0.4s here and there.
Yeah, the sats curves are much smoother in the diagnostic studies.
StillAnotherGuest wrote: split_city wrote:I have a question for you:
Just say the below "event" lasted >10secs and sats dropped by >3%, would it be called a hypopnea or apnea?
An apnea. The new rules say >90% reduction in thermal flow, without regard to any desaturations. However, use of 3% as a desat is an accepted alternative definition for hypopneas (4% is recommended).
Coll, thanks for that. When was this new rule introduced and who introduced it?
Now when you say at least 90% reduction, are you referring to the breaths prior to the event or "baseline" breaths i.e. at the beginning of the study when the subject was awake. I ask because flow can be quite high in patients who cycle through events very quickly (like the examples I have given). Patient arouses and hyperventilates, due to increased drive, falls alseep and has an apea within a few breaths. This flow is much higher compared to baseline breathing at the start of the study.
StillAnotherGuest wrote:split_city wrote:StillAnotherGuest wrote:A 53 cmH2O swing during "normal" breathing?
Just how beefy is this guy?
SAG
Yep, those values are correct. I wouldn't call it "normal" breathing as he was quite flow limited. His airway was acting like a Starling resistor. Drive was very much increased!
All my subjects are obese. His BMI was around 32
A question I have then regarding the "swing" is not the 33 cmH2O nadir but the 20 cmH2O positive inflection. Exhalation is passive, even in OSA, so baseline
Pes is normally 0 cmH2O. I imagine with massive forces on the airway, you could require large positive pressures for exhalation, but that wouldn't be obstructive apnea, that would be obstructed airway requiring tracheostomy. Asthma might show high
Pes on exhalation, but the expiratory limbs of the waveform are not prolonged. Or, are you doing the compressed abdomen thing.
Basline Pes e.g. at FRC is not normally 0cmH20 when the individual is either upright or supine. When upright, Pes at FRC is negative due to the elastic recoil of the lungs. However, it's generally positive when an individual is in the supine position because medialstinal structures compress the oesophagus, thus compressing the oesophageal balloon. Most of my baseline values have been between 5-10cmH20. Now, the 20cmH20 you are seeing is at peak expiration, not FRC. You would expect Pes to go up a bit during expiration due to the action of the respiratory muscles. However, as I said previously, drive was increased in this patient. This drive was transmitted to to abdominal muscles. These muscles are generally pretty silent during "normal" breathing. However, they tend to crank up during increased drive and contract during
expiration. You can tell this to be the case because gastric pressure was increasing during expiration (towards the end of the apneas) in my very first picture I put up. This increased contraction of the abdominal muscles during expiration also contributes to the raised expiratory Pes.
I do perform
lung function tests on all my patients. This patient had a normal
lung function.
_________________
CPAPopedia Keywords Contained In This Post (Click For Definition):
Hypopnea
_________________
CPAPopedia Keywords Contained In This Post (Click For Definition):
Hypopnea
_________________
CPAPopedia Keywords Contained In This Post (Click For Definition):
Hypopnea
This Is A Different Subgroup...
Posted: Fri Oct 26, 2007 4:16 am
by StillAnotherGuest
split_city wrote:Well that's where the confusion lies as I was referring to the other snapshot when talking about the apnea
Yeah, there's starting to be too many patients.
split_city wrote:When upright, Pes at FRC is negative due to the elastic recoil of the lungs.
The effect, if any, of the elastic recoil of the lungs would be reflected as positive in
Pes.
split_city wrote:However, it's generally positive when an individual is in the supine position because medialstinal structures compress the oesophagus, thus compressing the oesophageal balloon. Most of my baseline values have been between 5-10cmH20.
For those patients, you're going to have to account for that as artifact. That's not a respiratory variable.
split_city wrote:Now, the 20cmH20 you are seeing is at peak expiration, not FRC. You would expect Pes to go up a bit...
A bit yes. 20, no.
split_city wrote:However, as I said previously, drive was increased in this patient. This drive was transmitted to to abdominal muscles. These muscles are generally pretty silent during "normal" breathing. However, they tend to crank up during increased drive and contract during expiration. You can tell this to be the case because gastric pressure was increasing during expiration (towards the end of the apneas) in my very first picture I put up. This increased contraction of the abdominal muscles during expiration also contributes to the raised expiratory Pes.
The first screen
is more representative of
Pes. A
transient increase in
Pes activity (as well as
transient gastric pressure elevation during response to apnea) is noted.
BTW, can you put the pressure grid up for those?
But this guy
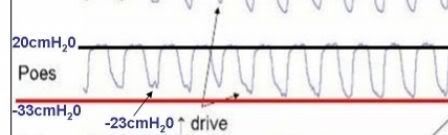
is very aggressively performing
active exhalation (+20 cmH2O) even during periods of "baseline" breathing. He'd need an enormous
Pcrit to have to do that, which would make him an "obstructed airway" patient rather than an "OSA" patient.
split_city wrote:When was this new rule introduced and who introduced it?
AASM earlier this year.
SAG
Well, I have to think about SOMETHING While I'm Running...
Posted: Fri Oct 26, 2007 7:06 am
by StillAnotherGuest
split_city wrote:I have a question for you:
Just say the below "event" lasted >10secs and sats dropped by >3%, would it be called a hypopnea or apnea? This has happened in a couple of my patients in that there was no inspiratory flow but very small expiratory flow. I can confirm no inspiratory flow as I was in the room watching and listening to the patient during some of these types of events. I could only hear a small "expiratory" snore.

While one would be tempted to say, "How can you continue to exhale without inhaling?", the answer is you can't, at least for very long anyway. Your aforementioned Starling principle (which occurs during inhalation) says that although flow becomes fixed, you still have flow. However, this applies only to flow limitations and hypopneas.
During an apnea, a new Starling curve is created, one that results in flow = 0. Exhalation would be allowed, but not inhalation (as you describe) as a one-way valve is created.
As an aside, this type of patient would now be
below FRC.
SAG
Re: This Is A Different Subgroup...
Posted: Fri Oct 26, 2007 10:47 am
by split_city
StillAnotherGuest wrote:split_city wrote:When upright, Pes at FRC is negative due to the elastic recoil of the lungs.
The effect, if any, of the elastic recoil of the lungs would be reflected as positive in
Pes.
I'm still a bit rusty when it comes to compliance, elastic recoil etc. In simple terms, FRC is the
lung volume at which the outward recoil of the chest is equal and opposite to the inward recoil of the
lung. Why is Pes negative at FRC? To understand why, I simply use an airfilled syringe. Please correct me if I'm wrong as this isn't my area, but I would love to learn. Think of the inside of the syringe as the lungs or esophagus while your hand represents the ribcage. Put your finger on top of the syringe and pull the plunger down and hold the plunger in place. Say this point is analagous to FRC i.e. the inward recoil (syringe/lungs) is balanced by the outward pull on the syringe (hand/chest). If you let go of the syringe, the syringe would recoil back. If you measure the pressure inside the syringe when you held the plunger in place, the value would be negative i.e. what it would be in the lungs at FRC.
StillAnotherGuest wrote:split_city wrote:However, it's generally positive when an individual is in the supine position because medialstinal structures compress the oesophagus, thus compressing the oesophageal balloon. Most of my baseline values have been between 5-10cmH20.
For those patients, you're going to have to account for that as artifact. That's not a respiratory variable.
Yep, I understand that this positive value is an artifact. Unfortunately, we cannot measure pleural pressure.
StillAnotherGuest wrote: split_city wrote:Now, the 20cmH20 you are seeing is at peak expiration, not FRC. You would expect Pes to go up a bit...
A bit yes. 20, no.
Ok, I have had a look at some other data from some of my other patients. During basal breathing when 1) drive is low and 2) no increase in Pga during expiration, peak Pes is around 5-10cmH20. However, patients with increased drive + Pga increases during expiration, had a peak Pes between 15-20cmH20. The patient with the 20cmH20 peak in Pes during high drive situations, only had a peak of around 10cmH20 during breaths under low drive conditions.
StillAnotherGuest wrote: split_city wrote:However, as I said previously, drive was increased in this patient. This drive was transmitted to to abdominal muscles. These muscles are generally pretty silent during "normal" breathing. However, they tend to crank up during increased drive and contract during expiration. You can tell this to be the case because gastric pressure was increasing during expiration (towards the end of the apneas) in my very first picture I put up. This increased contraction of the abdominal muscles during expiration also contributes to the raised expiratory Pes.
The first screen
is more representative of
Pes. A
transient increase in
Pes activity (as well as
transient gastric pressure elevation during response to apnea)
Ok, I won't draw them on the picture but this guy's peak Pes during his obstructive events (times when drive was high and Pga increased during expiration) was also between 15-20cmH20. His peak Pes during low drive conditions was around 5-8cmH20
StillAnotherGuest wrote:But this guy
is very aggressively performing
active exhalation (+20 cmH2O) even during periods of "baseline" breathing. He'd need an enormous
Pcrit to have to do that, which would make him an "obstructed airway" patient rather than an "OSA" patient.
Again, this is during a high drive state and hardly constitutes "baseline" conditions i.e. patent airway. His airway is acting as a starling resistor. His GG is active enough to prevent a full on obstructive event. Unfortunately, the Pga trace was lost during this period but I would bet he was cranking his abdominal muscles, thus increasing Pga, during this high drive state.
As I have pointed out, he wasn't the only one to show a peak Pes of around +20cmH20 during these high drive conditions.