palerider wrote:McSleepy wrote:Thus, the pressure exerted by the forced air acts to push the soft tissue lining those cavities against a solid foundation, and therefore does not depend on the ambient (atmospheric) pressure in the room.
no.
McSleepy wrote: What is often forgotten when talking about the efficiency of a CPAP therapy is the actual air flow produced influencing the therapeutic pressure: for a given machine-set pressure, the higher the flow - the lower the actual pressure on the tissues.
no. the air flow in your breathing passages is purely a function of your normal respiration, and is the same with or without cpap. increased cpap pressure does not result in faster airflow in your respiratory system.
though I'd be quite interested in the actual mathematical proof you're using to back up your claims.
Do you mathematically prove anything you say? Or just ask others to do it? Plus, this is not mathematics, it's physics. And basic physics, at that. The basis for my conclusions are rather fundamental and I'll lay out some of them here, but I don't intend to engage in a mindless argument. I don't even understand the statement you made, so I'm not really answering it, just explaining mine. This isn't about pride and I'm secure enough to not want to waste my time in proving myself. Maybe the student who asked the question would benefit from it, though, so here are the basics.
Pressure is a force that is distributed over a rigid surface. Only in the static case (no motion) is it evenly distributed, balanced and its value - constant, but it is, nonetheless, defined at all times. In the static case, if you apply a known pressure to a chamber (e.g., where the CPAP sensor is) connected to another chamber (your oral/nasal cavity) and want to know the pressure on the surface of that cavity, then you don't need to know anything else - that's the same pressure everywhere. The static case is realized when you have a rigid boundary and no change in mass (constant volume and no addition or subtraction of air; temperature, too, but let's not get into thermodynamics). As an example, If you connect the CPAP machine to a glass bottle, you can rest assured that the pressure inside would be exactly the same as the gauge reads and would not be affected at all by ambient pressure as the latter is fully balanced by the rigid body of the bottle (and so is the inner pressure, delivered by the CPAP); they are simply not allowed to interact with each other. The model of the human oral/nasal cavity is close enough to the bottle (the skull is rigid) when you are not breathing (between breaths). In the dynamic case the pressure over the boundaries can vary from, say, the inlet pressure, and across the boundary itself, but it still would not be affected by the pressure outside the boundaries, as long as those are rigid, for the same reasons. If the boundaries were not rigid, then there would be some variation from yield but unless those boundaries vary a lot, it would not be significant. In this case we may not know the exact value of the pressure inside the chamber (cavity) but the latter is still not significantly affected by ambient pressure because none of the parameters are influenced by it. Now, I need to clarify something else. If we were talking about the measurement of the pressure values, we'd need to specify whether we are talking about absolute or relative pressure readings. The reading that the CPAP machine uses is a relative ("gauge") pressure, which is referenced to ambient, but the discussion has been about the effect of the physical conduits (masks, nose or mouth inlet), excluding the source, thus I have been discussing from an absolute standpoint; how you measure that is a different topic.
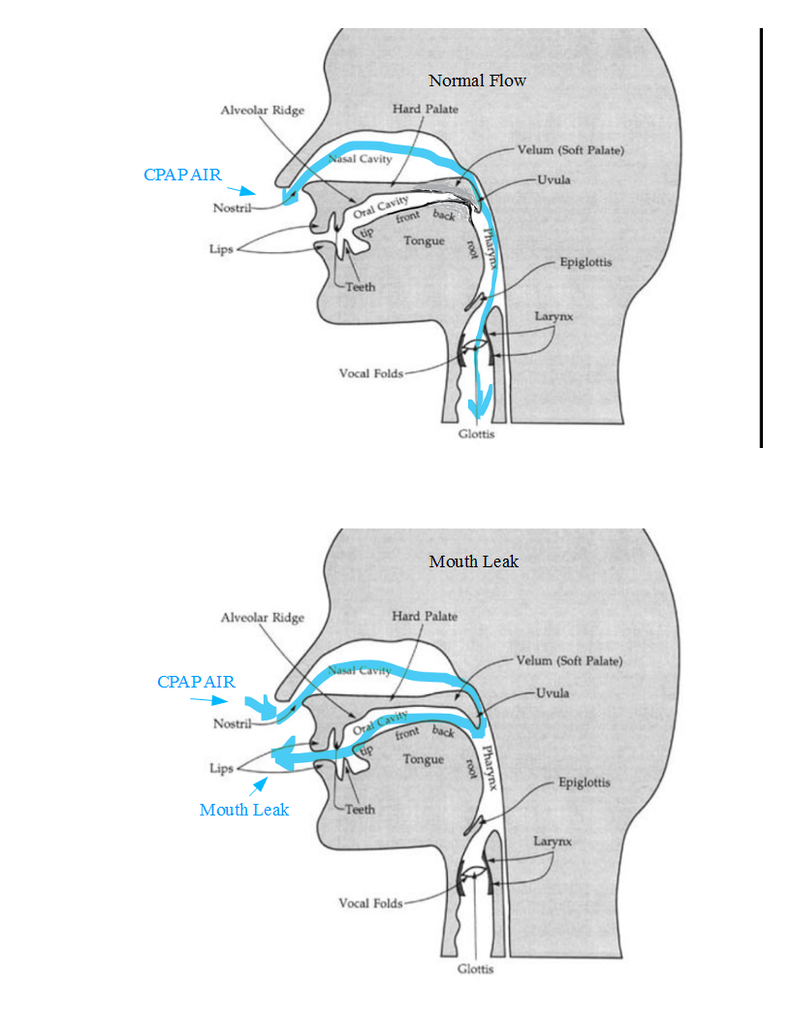
Looking at pressure variations in the dynamic case, though, it gets quite complicated. There are multiple aspects of it. One is if the boundaries are moving (e.g., lungs/diaphragm expanding and contracting), but since the oral/nasal cavities are on the conduit and not the reservoir, what matters is the flow of air. As you inhale and exhale the air flows quite briskly in and out through the air passages. And the pressure varies widely with the flow. I'm not going to get into details about the Bernoulli's principle and the related Venturi effect (you can look it up), but as it relates to air/CPAP, it states that the pressure over the walls of a conduit (a more or less coherent flow field) varies in proportion (quadratic) to the flow speed. Thus, each narrowing of the conduit represents a drop in pressure. A person with a lesser section of their air passage where the soft tissue needs support by the CPAP would have lesser pressure, and thus - support - than a person with a larger section, at the same pressure settings delivered by the CPAP machine. The compressibility of air makes this more complicated, but what really makes it complicated is the large variations in time of that section within the same person: head/jaw/tongue position, swelling of tissue, etc., all make it so that the pressure where it matters varies significantly from what the machine delivers. Add to that a variety of other effects, such as the throttling of the airflow by the mouth/tongue opening, and nose structure (for nasal masks; deviated septum and enlarged turbinates are a good example), which act like pressure regulators before the airflow has reached the soft tissues, and you see how the pressure readings of the machine can be quite arbitrary. Luckily, it's all empirical and CPAP users figure it out one way or another. Also, some people are affected more than others. The aforementioned nasal-passage blockages are a big factor for some, while those with nice, open air-passages don't really feel those effects. I know I didn't have any such problems and could use much lower pressures when I tried using an oral mask (Oracle; wish I could be using it), but are very sensitive to variations, and use very high pressures with my nasal-pillow mask.
I hope this makes it clearer.
McSleepy