Snoredog, just to let you know that I'm definitely not ignoring your comments! As usual I'm soaking your interpretations in since you "nail it" so often.
However, I'm not so sure I agree with your REM conclusion. Not that yours is a wrong conclusion regarding REM. It's just that I think the amount of information available is inconclusive regarding how much REM Cathy incurred. But as a working theory or opinion, your REM statement works just fine for me! And I hold your other interpretive statements in similar positive regard as well.
________________________________________________________________
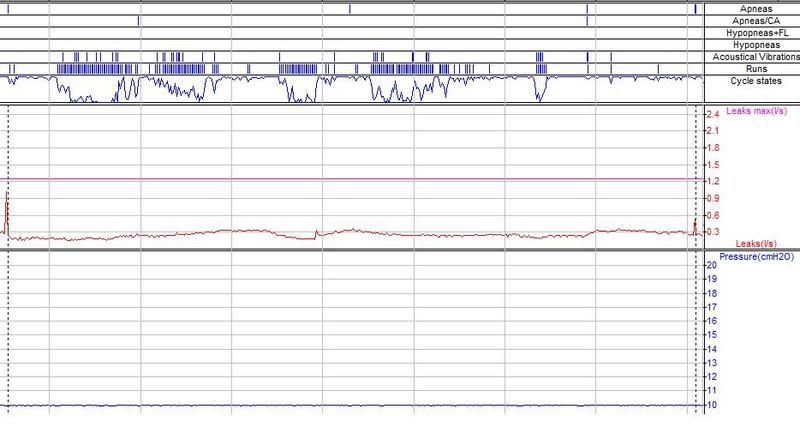
NightHawkeye wrote:tangents wrote:I respectfully disagree. This data looks much better to me than the chart on page 1 with the wide pressure range. ... I'm happy for you - to me it seems like you've made great progress!
Actually, I agree with you totally, Cathy. Communication is not my strong suit though , so I apologize for clumsy wording on my part. I think the data this morning looks like I may be closing in on the sweet spot, too!
Regards,
Bill
Cathy, thanks for pointing out that first-page chart!
Bill, I hope you're closing in on the sweet spot as well! But you just know we're all going to keep watching for potential calculation bugs, FL flare ups, mask-related measurement patterns, etc. It's that kind of stuff that's keeping us data-weenies riveted to this thread! But it's our hope for your improved health through better therapy that compels many of us to follow your threads in general!
__________________________________________________________________
Ozij, I find all your communications to be wonderfully thought-provoking.... Even if you do make our brains yell "ouch!" from time to time, exactly as Cathy humorously stated!
ozij wrote:I agree with 2 and 3 - not sure if I understand why this has to be a "regression type curve".
It doesn't have to be a regression type curve. I just glanced at it and thought:
"Hey! That sure looks kinda 'regression fitty' to me! But at that point I also suspected the cycle states graph is a best-fit curve among scattered points---with only three possible FL-related data-point values. I still lean toward thinking that...
ozij wrote: Patent no. 6,488,634 wrote:The determination of the degree of flow limitation present is based on four shape detection parameters, the sinusoidal index, the flatness index, the respiratory effort index and the relative flow magnitude index. The sinusoidal parameter or index is calculated as a correlation coefficient of the actual total inspiratory flow wave (filtered) to a reference sinusoidal half wave. As shown in FIG. 13, a half sinusoidal template 50 that matches the timing and amplitude of the actual total inspiratory flow data is compared to the actual total inspiratory flow data, for example, using a standard Pearson product moment correlation coefficient. This correlation coefficient is an index ranging from 1 (sinusoidal or not flow limited) to 0 (not sinusoidal).
If the actual total inspiratory flow data has less variable breaths, the correlation with a sinusoidal index drops, therefore all breaths will be given a lower sinusoidal index, etc. and there would be more flow limitations.
Well, what you have underlined in the patent description above refers to a correlation coefficient that exists only between: 1) the positive half of a sinusoid
template stored in firmware, and 2) the positive or inspiratory half of but
one respiratory cycle.
The measured inspiratory half of the cycle is comprised of sampled points that are statistically compared for variance against an idealized sinusoid template. That idealized sinusiod template is never anything other than a sinusoid---regardless of what Bill sets his pressure range to be. But the exact sinusoid used for comparison varies according to highly basic comparison parameters such as period, amplitude, volume. But here we always have one of many perfect sinusoid halves to compare against using Pearson.
And the other half of our covariance comparison is the
single measured inspiratory phase, which is Pearson sample-point compared against something that is always an idealized sinusoid half. But so far we're determining only probability index, P1. And we haven't even factored in other breaths. The Pearson coefficient exists only between a single measured breath and a single sinusoid template that is always a sinusoid.
Since this part of the calculation is independent of other breaths, and since the comparison template is always a sinusoid, I don't think the resulting Pearson correlation coefficient stands the potential to be impacted in any way by previous breaths that are not deemed sinusoidal.
There's plenty of potential for software bug in the overall probability equation, but I don't see how the Pearson calculation of P1 is impacted by previous breaths.
And I think you nicely pointed out yet a different part of the equation showing just that potential:
ozij wrote:Patent no. 6,488,634 wrote:FIG. 16 shows the prior probability factor which is applied to the initial value of the flow limitation parameter calculated from the shape parameters to yield a final value for the current valid breath. The prior probability factors are used to modify the flow limitation parameter based on previous breath's value for flow limitation. The underlined value is an estimate of the best value to be used as a multiplicative or additive to the index. Thus, the flow limitation parameter is made more important when other flow limited breaths have been detected. Similarly, the index is made less "flow limited" if the present occurrence is an isolated incident.
If the flow limitation parameter is between 1 and a predetermined normal reference value, e.g., 0.65-0.8, then the breath is classified as "normal." If the flow limitation parameter is between 0 and a predetermined flow limited reference value, e.g., 0.4, then the breath is classified as "flow limited." If the flow limitation parameter is between the normal and flow limited reference values, then the breath is classified as "intermediate."
By definition, we get a (calculated, albeit not valid) flow limitation cascade.
One of my initial thoughts as well. And I still suspect this part of the equation stands potential to be problematic.
However, we have that first semi-final probability calculation based on index 1 through index four. I'll call that Psub versus the probability calculation we finally end up with after index five steps in with it's temporal or context weighting. I'll just call that last one Pfinal for the sake of discussion.
If what you have underlined in red above uses
previous Pfinal values in its calculations (as opposed to using Psub),
then we have a
massive potential for cascade IMO. I would expect this type of data-return cascade to be even more rampant than what we see in this thread. On the other hand maybe this is
exactly what we're seeing on these data charts! Or maybe we're seeing epidemiologically skewed B-coefficient weightings that render final probabilities incorrect under certain index combinations. Perhaps we're seeing the accumulative skew of three or four indexes, each barely leaning toward FL-positive---when the overall inspiratory curve is not quite problematic or even genuinely FL (Bill, a problematic unidirectional-leaning of multiple parameters, very similar to "tolerance stacking" issues in engineering).
If, on the other hand, index five employs
previous Psub values in its temporal or context comparison weighting (as opposed to relying on previous Pfinal values),
then I think we see a
much more potentially viable method of weeding out the likes of isolated signal noise and measurement artifacts.