What if you have mostly hypnopeas and not apneas?
What if you have mostly hypnopeas and not apneas?
I'm still horribly tired from CPAP (more than before tx) and was just cleaning out my desk and found and re-read my copy of my PSG.
A few things lend me to think that my dx of severe OSA may have been overstated:
Total sleep time 286 minutes.
SaO2% desat:
>= 2 (time below 95%) = 4:35 minutes (I assume this is is wrong and actually means 4 hours and 35 minutes)
>= 3 (time below 90%) = 40 minutes
>= 4 (time below 85%) = 37 seconds
Heart rate (%)
80-71 0.62
70-51 13.9
60-51 77.5
50-41 7.03
Now is this dessat level and increase in heart rate really that bad???
Next, AHI ot 56.4, with RDI (including RERA's of 54.6). However there were 25 obstructive hypopneas, 1 central, and 241 hypnopeas. S, there were 10 TIMES as many hypnopeas as apneas! So in my view I don't really have
OSA but OSH(??). IOW 10 times as many hypnopneas as apneas.
So I don't understand how I could be diagnosed with severe OSA when I only have I only had 25 true apneas over 5 hours>??
The only thing that really concerns me is that there was no stage 3 sleep recorded, and also that 56.4 / hr respiratory arousals were scored, but then again I was in a sleep lab, so I would suppose that
the lack of stage three is meaningless, and frequent arousals would be much more likely than if I were sleeping at home, since obviously we don't sleep as well in a sleep lab as we do at home.
Any ideas anyone? My primary doctor (PCP in US) is of the opinion that the O2 sat is the primary marker for the severity of OSA (or OSH in my case).
But is 3% below awake saturation (excluding the 37%) really that bad??
I also noticed that the summary was not signed by an MD (I'm in the USA). I wonder if it would be possible to get a referral to a sleep specialist
to review the results.
The only thing that makes me take this lab result seriously is that they marked such frequent respiratory arousals.
For those of you who have better things to do than hang on this board all the time, I'm one of the ones who have felt worse since starting CPAP.
Larry
A few things lend me to think that my dx of severe OSA may have been overstated:
Total sleep time 286 minutes.
SaO2% desat:
>= 2 (time below 95%) = 4:35 minutes (I assume this is is wrong and actually means 4 hours and 35 minutes)
>= 3 (time below 90%) = 40 minutes
>= 4 (time below 85%) = 37 seconds
Heart rate (%)
80-71 0.62
70-51 13.9
60-51 77.5
50-41 7.03
Now is this dessat level and increase in heart rate really that bad???
Next, AHI ot 56.4, with RDI (including RERA's of 54.6). However there were 25 obstructive hypopneas, 1 central, and 241 hypnopeas. S, there were 10 TIMES as many hypnopeas as apneas! So in my view I don't really have
OSA but OSH(??). IOW 10 times as many hypnopneas as apneas.
So I don't understand how I could be diagnosed with severe OSA when I only have I only had 25 true apneas over 5 hours>??
The only thing that really concerns me is that there was no stage 3 sleep recorded, and also that 56.4 / hr respiratory arousals were scored, but then again I was in a sleep lab, so I would suppose that
the lack of stage three is meaningless, and frequent arousals would be much more likely than if I were sleeping at home, since obviously we don't sleep as well in a sleep lab as we do at home.
Any ideas anyone? My primary doctor (PCP in US) is of the opinion that the O2 sat is the primary marker for the severity of OSA (or OSH in my case).
But is 3% below awake saturation (excluding the 37%) really that bad??
I also noticed that the summary was not signed by an MD (I'm in the USA). I wonder if it would be possible to get a referral to a sleep specialist
to review the results.
The only thing that makes me take this lab result seriously is that they marked such frequent respiratory arousals.
For those of you who have better things to do than hang on this board all the time, I'm one of the ones who have felt worse since starting CPAP.
Larry
_________________
| Mask: FlexiFit HC407 Nasal CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
-- Speep study---
AHI = 56.4, RDI = 56.4
breakdown: 5.9 apnea, 0.2 central, 50.6 hyponpea, avg duration 20 sec.
AHI back=77.7, side=0.8 prone = 58.2
O2 desat min 83%, 40.3 min or desat < less then 91%
AHI = 56.4, RDI = 56.4
breakdown: 5.9 apnea, 0.2 central, 50.6 hyponpea, avg duration 20 sec.
AHI back=77.7, side=0.8 prone = 58.2
O2 desat min 83%, 40.3 min or desat < less then 91%
Re: What if you have mostly hypnopeas and not apneas?
From this link -- http://www.clevelandclinicmeded.com/med ... breathing/ comes this definition of Obstructive Sleep Apnea-Hypopnea Syndrome (OSAHS):
apnea - total cessation of airflow for at least 10 seconds, and
hypopnea - a 10-second event during which there is continued breathing but in which ventilation during sleep is reduced by at least 50% from baseline
Note also the diagnostic standard - For sleep-disordered breathing to be diagnosed as OSAHS, the patient must have at least five obstructed breathing events per hour (or 30 events per 6 hours of sleep). These events can be a combination of OSA, hypopnea, or respiratory effort-related arousals.
From the CPAPWiki (wiki/index.php/Apnea_Hypopnea_Index), it indicates that your AHI of 56.4 exceeds the clinical standard for a diagnosis of "Severe" OSAHS.
In terms of O2 levels, my sleep doc and primary doc both told me that so long as the SPO2 levels are at 88% or higher, there is nothing to worry about. Like you, I often have brief periods each night where I drop below that 88% threshold, and my docs have reviewed the reports and not indicated any concerns.
FWIW
Note the definitions for:Definition
OSAHS is characterized by recurrent episodes of partial or complete airway obstruction during sleep due to repetitive collapse of the pharynx, necessitating recurrent awakenings or arousals to re-establish airway patency. This airway obstruction or partial obstruction manifests in a reduction in airflow, termed hypopnea, or in a complete cessation of airflow, termed apnea, despite ongoing inspiratory effort. Hypopnea is defined in adults as a 10-second event during which there is continued breathing but in which ventilation during sleep is reduced by at least 50% from baseline. Apnea is total cessation of airflow for at least 10 seconds. Apnea can be obstructive or central. Obstructive apnea is defined as cessation of airflow but with continued respiratory effort, whereas central apnea is a state in which airflow and respiratory effort are both absent. Apnea also can be both central and obstructive, although obstructive apnea is more common. Hypopnea can produce clinical sequelae similar to those of apnea, but in general, apnea may be associated with a greater fall in oxygen saturations.
For sleep-disordered breathing to be diagnosed as OSAHS, the patient must have at least five obstructed breathing events per hour (or 30 events per 6 hours of sleep). These events can be a combination of OSA, hypopnea, or respiratory effort-related arousals. The patient must also have either excessive daytime sleepiness or at least two of choking or gasping from sleep, recurrent awakenings from sleep, feeling unrefreshed after sleep, daytime fatigue, or poor concentration. This second group of signs and symptoms must not be better explained by other factors. 2
The RDI (or AHI) is the number of apneas plus hypopneas per hour of sleep. This index has now become the standard by which to define and quantify the severity of OSAHS. An RDI of greater than 15 events per hour indicates possible OSAHS. Generally, as the RDI increases, the severity of apnea increases.
apnea - total cessation of airflow for at least 10 seconds, and
hypopnea - a 10-second event during which there is continued breathing but in which ventilation during sleep is reduced by at least 50% from baseline
Note also the diagnostic standard - For sleep-disordered breathing to be diagnosed as OSAHS, the patient must have at least five obstructed breathing events per hour (or 30 events per 6 hours of sleep). These events can be a combination of OSA, hypopnea, or respiratory effort-related arousals.
From the CPAPWiki (wiki/index.php/Apnea_Hypopnea_Index), it indicates that your AHI of 56.4 exceeds the clinical standard for a diagnosis of "Severe" OSAHS.
In terms of O2 levels, my sleep doc and primary doc both told me that so long as the SPO2 levels are at 88% or higher, there is nothing to worry about. Like you, I often have brief periods each night where I drop below that 88% threshold, and my docs have reviewed the reports and not indicated any concerns.
FWIW
-
RDawkinsPhDMPH
- Posts: 77
- Joined: Fri Dec 03, 2010 7:15 pm
- Location: Pensacola, FL
- Contact:
Re: What if you have mostly hypnopeas and not apneas?
As stated, the definition of obstructive sleep apnea syndrome counts hypopneas equal with apneas. For reasons not worth the space here: for all intents and purposes a hypopnea is as bad for your health as an apnea. I even won a Medicare hearing on this back in the early nineties when Medicare didn't normally recognize hypopneas.
As for the O2, I totally disagree with your PCP that O2 is the primary determinant of the severity of your apnea. It is usually, in my opinion, an important secondary indicator of the severity. Just my humble opinion.
As for the O2, I totally disagree with your PCP that O2 is the primary determinant of the severity of your apnea. It is usually, in my opinion, an important secondary indicator of the severity. Just my humble opinion.
Re: What if you have mostly hypnopeas and not apneas?
RD,RDawkinsPhDMPH wrote: As for the O2, I totally disagree with your PCP that O2 is the primary determinant of the severity of your apnea. It is usually, in my opinion, an important secondary indicator of the severity. Just my humble opinion.
Maybe you could expound on the O2 data/metric uses over in this topic -- viewtopic/t58315/PulseOxygen-Metrics.html as well??
Re: What if you have mostly hypnopeas and not apneas?
OK, good point about the O2 level. I can see where where frequent awakenings, for example, without and O2 drop, can cause health problems.RDawkinsPhDMPH wrote:As stated, the definition of obstructive sleep apnea syndrome counts hypopneas equal with apneas. For reasons not worth the space here: for all intents and purposes a hypopnea is as bad for your health as an apnea. I even won a Medicare hearing on this back in the early nineties when Medicare didn't normally recognize hypopneas.
As for the O2, I totally disagree with your PCP that O2 is the primary determinant of the severity of your apnea. It is usually, in my opinion, an important secondary indicator of the severity. Just my humble opinion.
But excuse me, but part of my question implicitly asked if a hypnopnea is comparable to an apnea in terms of negative health consequences.
And your answer it is that it is is just as bad for you. But yet you state "for reasons not worth the space" you won't explain why.
So, I asked a question, and basically you didn't answer it, but just stated an unfounded opinion.
It if is not worth the space to answer on this forum, then please respond by PM, or better yet, simply post a link to to the relevant research papers.
Oh by the way, did you know that for reasons not worth the space here: the moon is made of chocolate? Unfortunately, there is not enough space here to explain the reasoning, so I trust you will take this as fact.
Best Regards
_________________
| Mask: FlexiFit HC407 Nasal CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
-- Speep study---
AHI = 56.4, RDI = 56.4
breakdown: 5.9 apnea, 0.2 central, 50.6 hyponpea, avg duration 20 sec.
AHI back=77.7, side=0.8 prone = 58.2
O2 desat min 83%, 40.3 min or desat < less then 91%
AHI = 56.4, RDI = 56.4
breakdown: 5.9 apnea, 0.2 central, 50.6 hyponpea, avg duration 20 sec.
AHI back=77.7, side=0.8 prone = 58.2
O2 desat min 83%, 40.3 min or desat < less then 91%
-
RDawkinsPhDMPH
- Posts: 77
- Joined: Fri Dec 03, 2010 7:15 pm
- Location: Pensacola, FL
- Contact:
Re: What if you have mostly hypnopeas and not apneas?
Will do... it might be Monday before I have time to sit down and do it .... it will probably be on the thread DHC suggested. Feel free to PM me if I'm too slow getting to it for you.
Re: What if you have mostly hypnopeas and not apneas?
Absolutely. The massive Sleep Heart Health Study (SHHS) noted thatlarry63 wrote:My primary doctor (PCP in US) is of the opinion that the O2 sat is the primary marker for the severity of OSA (or OSH in my case).
Specifically, the frequency of hypopneas defined by a threshold of oxyhemoglobin desaturation of at least 4% was associated with cardiovascular disease. The strength or precision of association was not improved by reducing the desaturation threshold criterion to less than 4% or by including arousals in the definition.
"Don't Blame Me...You Took the Red Pill..."
- SleepingUgly
- Posts: 4690
- Joined: Sat Nov 28, 2009 9:32 pm
Re: What if you have mostly hypnopeas and not apneas?
larry63, Dr. Dawkins must have the patience of a saint that he's still willing to respond to you after the way you responded to him!
On my sleep study, I did not have desaturations. I was told that from what we know , the cardiovascular risks are associated with the desaturations; however, we don't know much about the impact on the brain. We do know that people that have these problems, even without desaturations, have a variety of maladies, such as EDS, cognitive dysfunction, anxiety, depression, functional somatic/pain disorders, etc. In short, the quality of life can be terrible, even with no desaturations. And I can personally attest to that!
On my sleep study, I did not have desaturations. I was told that from what we know , the cardiovascular risks are associated with the desaturations; however, we don't know much about the impact on the brain. We do know that people that have these problems, even without desaturations, have a variety of maladies, such as EDS, cognitive dysfunction, anxiety, depression, functional somatic/pain disorders, etc. In short, the quality of life can be terrible, even with no desaturations. And I can personally attest to that!
_________________
| Mask: Swift™ FX For Her Nasal Pillow CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Rescan 3.10 |
Never put your fate entirely in the hands of someone who cares less about it than you do. --Sleeping Ugly
Re: What if you have mostly hypnopeas and not apneas?
larry63,
A quick question, if I may.
I believe that you mainly or only had hypopneas during your sleep study.
And you're now using an S9.
On a typical night, does the S9 record more hypopneas or more apneas?
In other words, is the AI higher or is the HI higher? If you only have the data off the LCD, the HI = AHI - AI.
Thanks,
robysue
A quick question, if I may.
I believe that you mainly or only had hypopneas during your sleep study.
And you're now using an S9.
On a typical night, does the S9 record more hypopneas or more apneas?
In other words, is the AI higher or is the HI higher? If you only have the data off the LCD, the HI = AHI - AI.
Thanks,
robysue
_________________
| Machine: DreamStation BiPAP® Auto Machine |
| Mask: Swift™ FX Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: PR System DreamStation and Humidifier. Max IPAP = 9, Min EPAP=4, Rise time setting = 3, minPS = 3, maxPS=5 |
-
RDawkinsPhDMPH
- Posts: 77
- Joined: Fri Dec 03, 2010 7:15 pm
- Location: Pensacola, FL
- Contact:
Re: What if you have mostly hypnopeas and not apneas?
Darn ... Sorry ... I just wrote a long (for me) reply, even agreed with NotMuffy somewhat ... but lost it, I apparently wasn't logged in
I'll rewrite, but I have to do some work, so it might be awhile and it might not be as eloquent as the original.
I'll rewrite, but I have to do some work, so it might be awhile and it might not be as eloquent as the original.
-
RDawkinsPhDMPH
- Posts: 77
- Joined: Fri Dec 03, 2010 7:15 pm
- Location: Pensacola, FL
- Contact:
Re: What if you have mostly hypnopeas and not apneas?
So let me try again. First, the Disclaimer: (1) Nothing I say is meant to imply that oxygen levels and desaturations are not important, only that apnea, per se, even without desaturations can be bad for your health. and (2) Significant desaturations associated with the respiratory events of OSAS are the most acutely dangerous component of the disease.
The OP raised the question of whether having mostly hypopneas was different, from a health effect standpoint, than having mostly apnea and also stated that his PCP considered the desats the primary determinant of the severity of OSAS. My response was that the severity of OSAS is normally based on the AHI and that the desaturation was an important additional factor.
NotMuffy, the data you present is relevant and useful. However, it was the frequency of events that was correlated with cardiovascular risk and "The strength or precision of association was not improved by reducing the desaturation threshold..." ... not some measure of desaturation such as area under the desaturation curve (inverse of the oximetry) or deepest or "average" desaturation. In fact, reducing the desaturation threshold or including arousals instead would be expected to reduce the accuracy and precision of event recognition resulting in greater data variability and, therefore, a reduced statistical association. This is why there is no desaturation requirement to score an apnea.
The pathophysiology of OSAS is complex and multifactorial and includes: "intermittent hypoxia leading to increased oxidative stress, systemic inflammation, and sympathetic activity; intrathoracic pressure changes leading to excessive mechanical stress on the heart and large artery walls; and arousal-induced reflex sympathetic activation with resultant repetitive blood-pressure rises." Kohler & Stadling, Nat Rev Cardiol, 2010, 7(12):677-85. But even the effect of intermittent hypoxemia is open to debate: "extensive evidence in animals and humans has shown controlled intermittent hypoxia conditioning programs to be safe, efficacious modalities for prevention and treatment of hypertension." Serebrovskaya, et al., Exp Biol Med, 2008, 233(6): 627-50. It is possible, maybe even probable, that the various effects of sleep apnea have different primary causes/predictors. "Vascular responses may be more directly related to sympathetic surges and arousals, whereas metabolic sequelae may be mediated more by hypoxic stress." Sulit, et al., Sleep, 2006, 29(6): 777-83. And finally, the relationship between the respiratory event and the degree of desaturation, while conceptually straightforward, involves more parameters than most OSAS sufferers realize. (Dr Andrew Chesson gave an excellent presentation of this about 15 yrs ago at, I think, the Southern Sleep Society.)
This has practical implications. Frequently, a newly diagnosed OSAS sufferer will ask if O2 by nasal cannula would be acceptable and, sometimes, their physician may accommodate them by prescribing such. Although supplemental O2 may blunt some of the detrimental effects of OSAS, the body of evidence suggests that it will be less efficacious than CPAP. Also, simple oximetry can sometimes provide supportive data of the diagnosis of OSAS, it cannot reliably prove the absence of apnea. And the relevance of the data mentioned by NotMuffy is in policy: the diminshing returns to be had in the commitment of financial resources to treat OSAS in a subgroup for which the data is less reliable.
Furthermore, research in recent years has begun to elucidate the association between sleep and metabolic energy balance. This data begins to explain the results of sleep deprivation studies done by Dr Allan Rechtschaffen in the 1980's. It is possible that the effect of respiratory event related arousals will again gain importance, this time as an important target in the management of obesity.
So returning to the OP. The question was: (a) does it matter that it was mostly hypopneas? That is what I beat Medicare on almost 20 years ago. The simple answer is that the accepted definition of OSAS does not distiguish between apneas and hypopneas in the diagnosis. (b) is O2 desat the primary determinant of OSAS severity? The simple answer is that is not the accepted standard of the sleep community.... the further questions that came up on this board (this is my interpretation of the posts) include: (c) does the desat level matter? And the answer is, without question, yes. (d) do respiratory events without desaturations (let's define desaturation as greater than 3 percentage points) matter? And my answer, and I think you can see I'm not alone, is yes. And this goes beyond the potential hypersomnolence because of sleep disruption hypothesis. (In fact, the correlation between hypersomnolence and AHI and/or arousals is not as tight as you might think.)
I hope this helps. I will be happy to respond to any debate, time permitting.
The OP raised the question of whether having mostly hypopneas was different, from a health effect standpoint, than having mostly apnea and also stated that his PCP considered the desats the primary determinant of the severity of OSAS. My response was that the severity of OSAS is normally based on the AHI and that the desaturation was an important additional factor.
NotMuffy, the data you present is relevant and useful. However, it was the frequency of events that was correlated with cardiovascular risk and "The strength or precision of association was not improved by reducing the desaturation threshold..." ... not some measure of desaturation such as area under the desaturation curve (inverse of the oximetry) or deepest or "average" desaturation. In fact, reducing the desaturation threshold or including arousals instead would be expected to reduce the accuracy and precision of event recognition resulting in greater data variability and, therefore, a reduced statistical association. This is why there is no desaturation requirement to score an apnea.
The pathophysiology of OSAS is complex and multifactorial and includes: "intermittent hypoxia leading to increased oxidative stress, systemic inflammation, and sympathetic activity; intrathoracic pressure changes leading to excessive mechanical stress on the heart and large artery walls; and arousal-induced reflex sympathetic activation with resultant repetitive blood-pressure rises." Kohler & Stadling, Nat Rev Cardiol, 2010, 7(12):677-85. But even the effect of intermittent hypoxemia is open to debate: "extensive evidence in animals and humans has shown controlled intermittent hypoxia conditioning programs to be safe, efficacious modalities for prevention and treatment of hypertension." Serebrovskaya, et al., Exp Biol Med, 2008, 233(6): 627-50. It is possible, maybe even probable, that the various effects of sleep apnea have different primary causes/predictors. "Vascular responses may be more directly related to sympathetic surges and arousals, whereas metabolic sequelae may be mediated more by hypoxic stress." Sulit, et al., Sleep, 2006, 29(6): 777-83. And finally, the relationship between the respiratory event and the degree of desaturation, while conceptually straightforward, involves more parameters than most OSAS sufferers realize. (Dr Andrew Chesson gave an excellent presentation of this about 15 yrs ago at, I think, the Southern Sleep Society.)
This has practical implications. Frequently, a newly diagnosed OSAS sufferer will ask if O2 by nasal cannula would be acceptable and, sometimes, their physician may accommodate them by prescribing such. Although supplemental O2 may blunt some of the detrimental effects of OSAS, the body of evidence suggests that it will be less efficacious than CPAP. Also, simple oximetry can sometimes provide supportive data of the diagnosis of OSAS, it cannot reliably prove the absence of apnea. And the relevance of the data mentioned by NotMuffy is in policy: the diminshing returns to be had in the commitment of financial resources to treat OSAS in a subgroup for which the data is less reliable.
Furthermore, research in recent years has begun to elucidate the association between sleep and metabolic energy balance. This data begins to explain the results of sleep deprivation studies done by Dr Allan Rechtschaffen in the 1980's. It is possible that the effect of respiratory event related arousals will again gain importance, this time as an important target in the management of obesity.
So returning to the OP. The question was: (a) does it matter that it was mostly hypopneas? That is what I beat Medicare on almost 20 years ago. The simple answer is that the accepted definition of OSAS does not distiguish between apneas and hypopneas in the diagnosis. (b) is O2 desat the primary determinant of OSAS severity? The simple answer is that is not the accepted standard of the sleep community.... the further questions that came up on this board (this is my interpretation of the posts) include: (c) does the desat level matter? And the answer is, without question, yes. (d) do respiratory events without desaturations (let's define desaturation as greater than 3 percentage points) matter? And my answer, and I think you can see I'm not alone, is yes. And this goes beyond the potential hypersomnolence because of sleep disruption hypothesis. (In fact, the correlation between hypersomnolence and AHI and/or arousals is not as tight as you might think.)
I hope this helps. I will be happy to respond to any debate, time permitting.
Last edited by RDawkinsPhDMPH on Tue Dec 21, 2010 8:33 am, edited 1 time in total.
Re: What if you have mostly hypnopeas and not apneas?
Thanks! Dovetails info I read today on brain inflammation and its effects.RDawkinsPhDMPH wrote:...
_________________
| Mask: Hybrid Full Face CPAP Mask with Nasal Pillows and Headgear |
| Humidifier: HumidAire H4i™ Heated Humidifier |
| Additional Comments: Started Aug '07 CPAP Escape at 11 then 9, S9 APAP range 9.8-16, now 10-17 |
ResMed S9 range 9.8-17, RespCare Hybrid FFM
Never, never, never, never say never.
Never, never, never, never say never.
Re:Tip
Tip for not loosing posts: compose them in Notepad, and then copy paste.
On this forum, if you inadvertantly leave the "compose" page -- you lose everthing you typed
O,
On this forum, if you inadvertantly leave the "compose" page -- you lose everthing you typed
O,
_________________
| Mask: AirFit™ P10 Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: Machine: Resmed AirSense10 for Her with Climateline heated hose ; alternating masks. |
And now here is my secret, a very simple secret; it is only with the heart that one can see rightly, what is essential is invisible to the eye.
Antoine de Saint-Exupery
Good advice is compromised by missing data
Forum member Dog Slobber Nov. 2023
Antoine de Saint-Exupery
Good advice is compromised by missing data
Forum member Dog Slobber Nov. 2023
Re: What if you have mostly hypnopeas and not apneas?
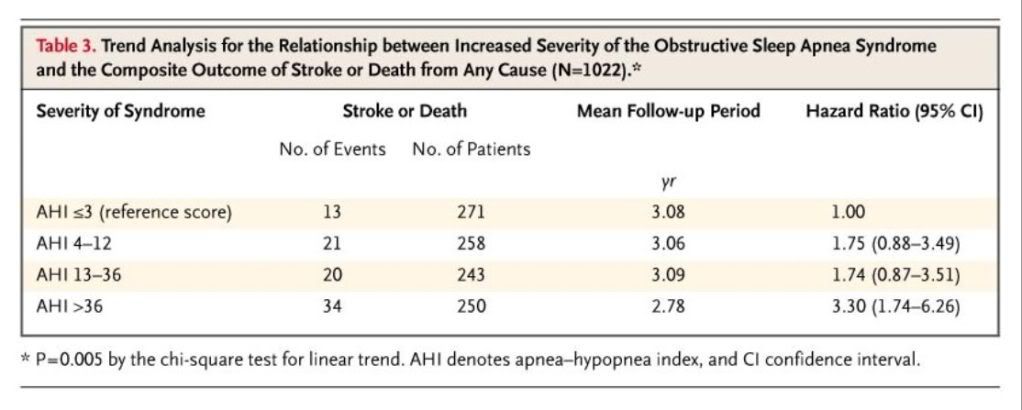
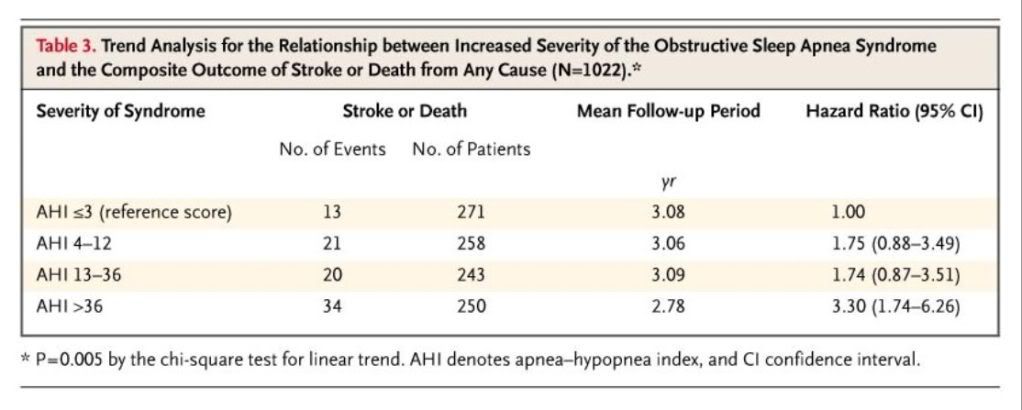
In another huge study, Yaggi et al (2005) looked at AHI and the risk of catastrophic events, and it became quite clear that severe OSAS (AHI > 36) was associated with much greater risk:
The scary part, however, was that these patients were being treated:
The scary part, however, was that these patients were being treated:
Many patients with the obstructive sleep apnea syndrome received some type of treatment for sleep apnea after the initial evaluation. Thirty-one percent achieved a weight reduction of 10 percent or more; 58 percent were using airway pressurization for at least four hours per night for five nights or more per week; 15 percent underwent upper-airway surgery.
"Don't Blame Me...You Took the Red Pill..."
-
RDawkinsPhDMPH
- Posts: 77
- Joined: Fri Dec 03, 2010 7:15 pm
- Location: Pensacola, FL
- Contact:
Re: What if you have mostly hypnopeas and not apneas?
Excellent paper ... again, the independent variable is AHI... not AI, not HI, and not any measure of desaturation....
It's unfortunate that they were not able to break down the data based on which OSAS therapy had been tried and whether there was documentation that it had worked.. but that's a later study.
What is interesting (and I thought there was earlier data on this, but I may be wrong) was that the correlation was independent of such known risk factors as hypertension.... in other words, as far as we can tell, sleep apnea itself increases your risk.
It's unfortunate that they were not able to break down the data based on which OSAS therapy had been tried and whether there was documentation that it had worked.. but that's a later study.
What is interesting (and I thought there was earlier data on this, but I may be wrong) was that the correlation was independent of such known risk factors as hypertension.... in other words, as far as we can tell, sleep apnea itself increases your risk.












