Morbius,Morbius wrote:Well, I'm going to disagree with just about everything there. My generalizations are:Machinehead wrote:I believe that RERAS are MORE disruptive than OSA. The problem with OSA people is that they usually maintain sleep. The defining characteristic of a RERA, is that there is always an arousal at the end of it. The majority of pts I see are Medicare, COPD. Its very Common to have an AHI of 5 and an RDI of 20-40. Its not a simple fix either. OSA, even at AHI's of 100+, pop the airway open, pt is fine. RERAS are much more difficult. You have to stabilize the airway, then open it a little. They usually require a much higher pressure. Just my opinion.
See http://jap.physiology.org/content/116/3/302 discussing the role of the arousal.
- OSA is more disruptive than UARS (low AHI/high RDI);
- OSA people do not maintain their sleep;
- COPD (moderate to severe anyway) have hypoventilation episodes and not UARS characteristics ("Overlappers");
- The fix for RERAs is not aggressive pressure attack ("The Krakow Kool-Aid"); and most importantly
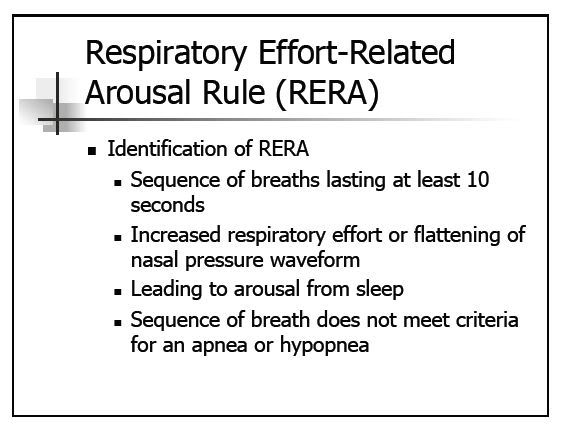
- While the defining characteristic of a RERA is that there is always an arousal at the end of it, one wonders if scorers and reviewers are really checking to see if that is the case.
In the case of FL, are you seeing some benign flow limitation, an arousal somewhere near there, and going "AHA! There's a RERA!", try to hammer it to death with pressure, and then conclude that when the patient finally gets to consistent sleep (passes out, really) at 57 cmH2O that high pressure is the key?
Or have you found a poor sleeper with a little nose, and now made sleep even harder?
I'm intrigued (as usual) about what you've added to the whole RERA/Flow limitation conversation.
I know you've looked at my own data in the past and have had a lot of things to say about it. Much of why I no longer bother worrying about my flow limitations is that what you've said in the past about benign flow limitations seems to "fit" me. And it's clear from previous experiments that no matter where I set my max IPAP limit, the machine will go there and the flow limitation index doesn't decrease very much, but my own restlessness and aerophagia problems will increase a whole, whole lot with an increase in the nightly pressure levels. And feeling lousy in the daytime comes with increased restlessness and increased aerophagia.
In other words, when I'm actually sleeping with the machine in terms of sleep efficiency and I'm remembering a minimum number of very short wakes, I now feel better than I did pre-CPAP, regardless of what my machine says about my flow limitations and RERAs.
And when I'm NOT actually sleeping with the machine---i.e. the sleep efficiency drops below about 80-58% and/or I wake up remembering a lot of short wakes and/or I wake up and have serious trouble getting back to sleep in the middle of the night, I feel just as lousy as I did back before the First War on Insomnia. And that lousy feeling is regardless of what my machine says about the AHI, the FLI, and the RERAs.
So I'd like to know more about what you refer to as benign flow limitations: What causes them? Is there any way for a mere PAPer to sort out whether the flow limitations they see in their data are benign flow limitations (that don't need more pressure) or are a significant factor in why their sleep is still not good (and additional pressure might be useful)?
Also if an APAP or an Auto bilevel responds aggressively to flow limitations, can the increased pressure in response to benign flow limitations cause more problems than it fixes? If so, is limiting the upper pressure setting and ignoring the flow limitation data a reasonable response?