I really would like to thank mellabella for the great explanation and example flow wave forms. Yes Upper Airway Resistance Syndrome (UARS) is a fight. The air flow flattens but if you look at the amount of vacuum in the esophagus you would find that each breath shows a bit more vacuum as the event proceeds. Respiratory effort can become great enough to warp the walls of the heart.
Most people think of sleep apnea only as obstructive sleep apnea. However there is a much broader spectrum of causes of apnea. As well the point at which arousal occurs with an event may well change. They are beginning to sort it out[2,3].
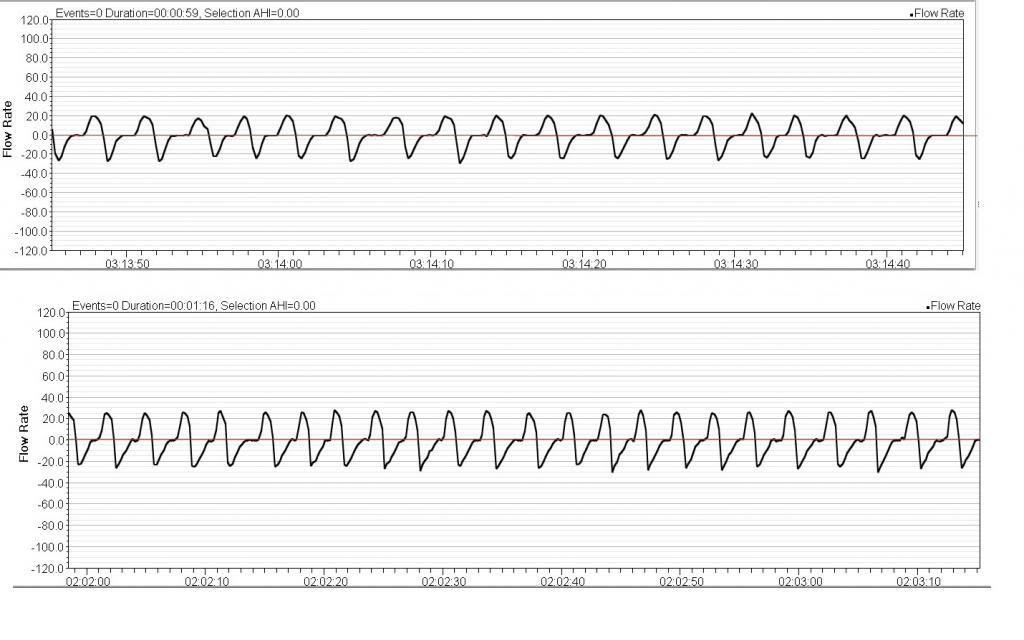
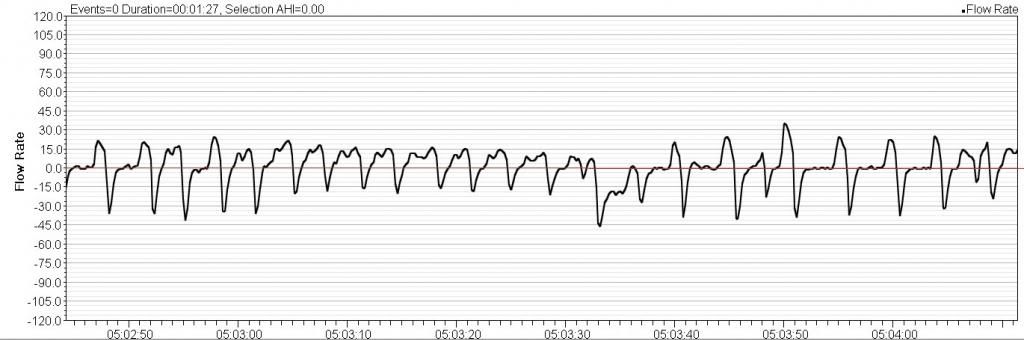
What I see in your graphs is a time of great respiration (much breathing) followed by an apnea. When you breath more you also wash out more carbon dioxide (CO2). In the context of hyopcapnic (hypo=low capnic=CO2) central apnea as the CO2 level decreases it goes beyond the “apneic threshold” and so the hypocapnic central apnea occurs.
From the over simplified world of Wikipedia:
http://en.wikipedia.org/wiki/Cheyne-Stokes_respiration Cheyne–Stokes respiration and periodic breathing are the two regions on a spectrum of severity of oscillatory tidal volume. The distinction lies in what is observed at the trough of ventilation: Cheyne–Stokes respiration involves apnea (since apnea is a prominent feature in their original description) while periodic breathing involves hypopnea (abnormally small but not absent breaths).
To me it looks like you show both a bit of Cheyne–Stokes respiration and periodic breathing in the flow waveforms provided. Since they did not find central apnea in the original study but we now see indications of it in your flow waveforms you may well be showing signs of CPAP emergent central apnea often known as Complex Sleep Apnea (CompSAS).
In terms of your being “constantly fatigued but my AHI looks good” I am suspicious that this results from two of the nonanatomic causes of sleep apnea[2,3] ganging up on you as you use CPAP. High respiratory control system gain working with low arousal threshold could mean that the times of more breathing brought forth by the respiratory gain issues would cause respiratory effort above your low arousal threshold and fracture your sleep with excessive arousals. In a recent comparison study looking at how CompSAS responds to treatment by ASV vs CPAP[1] they found that at the end of 90 days both arms were essentially equal in the number of arousals with over twenty per hour still in play. Both arms had excessive daytime sleepiness affected only a little by treatment. ASV however did well to severely reduce the hypocapnic central events so probably does better protect the brain.
I have found EERS[4] helpful to deal with this issue.
I and others[5] have found moving vitamin D3 into its active range helpful.
And during my journey away from sleep apnea I have found that I did not know how to eat well or move well. My three years with a dietitian helped start me on my continuing life long journey to eat well. I still strive toward the basic goal of 10,000 steps a day (running about 80% at this time) and do intend to use more personal trainer time as I pursue an active lifestyle. Lately I have been thinking that running, which is known to help with brain development, might well be worth the risks to my knees at my advanced age. By eating well and moving well I hope to promote whole body metabolic health and I can say it does appear to help with my tendency to have centrals emerge as I use CPAP.
hth
[1] Morgenthaler TI, Kuzniar TJ, Wolfe LF, Willes L, McLain WC, Goldberg R. The complex sleep apnea resolution study: a prospective randomized controlled trial of continuous positive airway pressure versus adaptive servoventilation therapy. SLEEP 2014;37(5):927-934 Related article (commentary):833
[2] Danny J. Eckert, David P. White, Amy S. Jordan, Atul Malhotra, and Andrew Wellman "Defining Phenotypic Causes of Obstructive Sleep Apnea. Identification of Novel Therapeutic Targets", American Journal of Respiratory and Critical Care Medicine, Vol. 188, No. 8 (2013), pp. 996-1004. doi: 10.1164/rccm.201303-0448OC
[3] Sairam Parthasarathy M.D., Emergence of Obstructive Sleep Apnea Phenotyping. From Weak to Strong! American Journal of Respitory and Critical Care Medicine VOL 188 2013
-- critical closing pressure [Pcrit] - Arousal Threshold - ventilatory control Loop gain - and genioglossal Muscle responsiveness. Pcrit, Loop, Arousal, Muscle (PALM)--
[4]: Gilmartin G, McGeehan B, Vigneault K, Daly RW, Manento M, Weiss JW, Thomas RJ.
Treatment of positive airway pressure treatment-associated respiratory instability with enhanced expiratory rebreathing space (EERS).
Source: J Clin Sleep Med. 2010 Dec 15;6(6):529-38. Division of Pulmonary, Critical Care and Sleep Medicine, Beth Israel Deaconess Medical Center, Boston, MA, USA.
Link:
http://www.ncbi.nlm.nih.gov/pubmed/21206741
[5]: Those who are working with the D3 hormone (A.K.A. Vitamin D3) (e.g. Dr. Stasha Gominak, Michael F. Holick, Ph.D., M.D., Vitamin D Council) seem to be finding that the very low side of the “normal” range of 30-100 ng/L produces a range of symptoms including OSA, pain, and infection. All believe that a level lower than 50 ng/mL is not good and Dr. Stasha Gominak recommends 60-80 ng/mL for good health. It would probably be wise to check your vitamin D3 levels. See “The Vitamin D Council” for assay details.