HELP AGAIN! ASV or APAP?
Re: HELP AGAIN! ASV or APAP?
Awesome another great piece of information and advice that I am going to look at tomorrow. I will most certainly ask for the raw data and/or if someone else can score the results. Thanks so far for the helpful information you have given me
_________________
| Mask: Quattro™ FX Full Face CPAP Mask with Headgear |
| Additional Comments: Trying my best to get quality rest. PR System ONE REMstar BiPAP Auto SV Advanced |
System One Respironics Bipap AutoSV Advanced Quattro Fx
Min EPAP: 13.0 CmH20
Min Pressure Support: 3.5
Max EPAP: 25.0
Max Pressure Support: 5.0
Max Pressure: 20.0
Flex Setting: Bi-Flex - 3
Backup Rate:Auto
Humidification Mode:off
Humidifier Setting:c5
Min EPAP: 13.0 CmH20
Min Pressure Support: 3.5
Max EPAP: 25.0
Max Pressure Support: 5.0
Max Pressure: 20.0
Flex Setting: Bi-Flex - 3
Backup Rate:Auto
Humidification Mode:off
Humidifier Setting:c5
Re: HELP AGAIN! ASV or APAP?
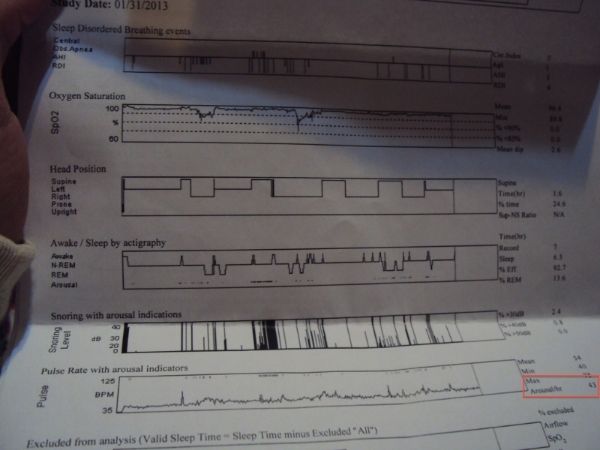
Yeah, now I see where 43 comes from. Note what OP's sleep doctor wrote in the last sentence of the 'sleep study findings' section, totally misleading interpretation.robysue wrote:Second page of the Home Sleep Study report clearly lists the AROUSALS/HOUR as 43. See the red rectangle in the (edited) version of sleepinow's Home Sleep Study report:musculus wrote: Also, I don't know why people say you got arousal index of 43 (that's very poor sleep), all I could see is 43 BPM event with index of 6 in your home study.
The red rectangle is at the FAR RIGHT of the page by the Pulse Rate with Arousals Indicators graph. That's why sludge and I have pointed out that there are a lot of (non respiratory related) arousals on this home sleep test.
That said, it's true that the home sleep doesn't have an EEG channel. They're using other data to infer when the arousals happened and whether the suspected arousals are related to sleep disordered breathing.
http://s14.postimg.org/8ba1aes7l/DSC05640.jpg
I guess 43/hr was higher than the true arousal index since heart rate will fluctuate in normal undisturbed sleep, also 43/hr will most likely make OP feel like a zombie during the day and have ZERO energy for exercise.
Re: HELP AGAIN! ASV or APAP?
So there are some significant differences in the conditions between the home sleep test and the lab tests that go beyond just "the lab tests were done in the lab".sleepinow wrote:If I can remember quite clearly. My home sleep test was done on my back and without any support to raise my body too far from the mattress. Something that I did the opposite on in the Split and ASV Titration Study. Basically I had two pillows underneath me with one half folded to given me an even bigger boost off the mattress.And I slept mostly on my sides. This is what makes me believe that I have less arousals as compared to the Home Sleep Study. I have self performed raising my body and sleeping on my sides to notice a significant difference in my sleep.4) Spontaneous arousals: On the diagnostic home sleep test, the arousal index was 43, meaning that approximately 43 times per hour the "surrogate arousal indicators" showed that it was likely you had an EEG arousal, even though there's no EEG data. An arousal is not quite the same a a full wake, but you can loosely think of an arousal as a sudden change from a deeper sleep stage to a lighter one. Most of the arousals on the home sleep test were NOT associated with sleep disordered breathing.
But it is odd that the number of spontaneous arousals---those that are NOT associated with respiratory problems---is so much greater on the in home sleep test than it is on the in-lab sleep tests. And the thing is, if you typically have this many arousals in your own bed, that could explain the continuing problems with daytime functioning. And so the question becomes, "How do you minimize the spontaneous arousals?" And I don't have an answer to that question.
Even so: On the ASV titration, there were 25 awakenings and 24 spontaneous arousals in spite of the ASV treatment. On the split test, there were NO spontaneous arousals on either part of the night, but there were 24 awakenings, most of which occurred during the diagnostic part of the night. So while the spontaneous arousal index on the in-lab tests may be less than the home sleep test, there's still an obvious problem with sleep continuity that doesn't seem to be associated with SDB.
So you had two exceptionally bad nights in the lab as far as getting and staying asleep are concerned. That means that it's really hard to get a sense of what's really going on with your sleep with or without the PAP. Which means that you still don't have a really good idea of just what's going on in your sleep, and hence you don't really know what (if anything) PAP can really do for you---regardless of whether its CPAP or an ASV machine.Yes! On my Split Study, I noticeably had trouble falling asleep because the darn sleep technician coughed every now and then waking me up. I was falling asleep and then I heard his cough which raised my anxiety and woke me up. He definitely had a cold or something. Now, I normally wear earplugs to bed because I am sensitive to noise. I forgot my good earplugs at home but I had some that were a bit above average/average in my car. So while it cancelled out many of the noises, I still heard him cough and I had somewhat anxiety because my mind was racing and replaying things like (Oh no, You do not have your earplugs (the good ones). Your not going to fall asleep. Is that noise that I heard?) Eventually though, I did feel like my anxiety dropped after about an our or two. I normally fall asleep really fast especially at home so I guess I did have a bit on a in-lab effect. I forgot to mention, that during the ASV titration (this is not the study taken with the bad earplugs) it was hot as hell! At least to me it was. I had to take most of the covers off. But by morning I was freezing my ass offThe home sleep test's total sleep time and sleep efficiency were actually pretty good. Now some of the differences could be lab effect---it is more difficult to get to sleep in a strange place.
andYes, I have personally tested myself many times doing this.And you've commented elsewhere that nights following days when you exercise are much worse in terms of sleep quality than nights following days you don't exercise.
So correct me if I'm wrong: You know you don't sleep well when you exercise, and so you exercised (a bit more than usual) before the in-lab sleep tests, which are known to be difficult because you're asked to sleep in a strange place with wires all over you and someone watching you all night long?Yes. During both the ASV Titration and Split Study, I did exercise but not too much. It was much more exercise than I usually do. (I usually have zero or near zero forms of exercise (I will not even lift or carry heavy things) every damn day except for the days I masterbate) But compared to other people, it is considered highly minimal. For example, on the ASV Titration Study, I changed all four of my tires and masterbated. And didn't exercise before others??? I do not remember the Home Sleep Study, but I would believe that I might have exercised there too because it was around that time where I actually did exercise like normal people exercise e.g running a mile or two and going to the gym. Overall I purposefully exercised more before the tests because it disrupts my sleep more because maybe it brings me to a more relaxed state when trying to sleep. I did this because I wanted a titration number that is in line with when I exercise, because I plan on exercising until I can no longer. But please note that I do not overexercise. It is weird but I think that since exercise is highly related to deep sleep, that it will trigger more apneas because it makes my throat more relaxed. But who knows?! Right?Which raises the side question: Do you happen to recall if you exercised before any of the sleep tests?
It's no wonder that you didn't get much sleep on those tests. And unfortunately the lack of sleep on those tests is, itself, a problem. For example, you never got into REM on the split night test and so there's no hard data about what your apnea might look like in REM sleep. Quite frankly it's a bit of a surprise to me that with only 75 minutes of sleep time during the diagnostic part of the sleep study that they bothered to wake you up and put a mask on you. Typically labs insist on at least 120 minutes of sleep during the diagnostic part of a split study to move onto the titration part of the test.
So I still think you need an accurate diagnosis for your sleep problems. It's not clear if you have a sleep disordered breathing problem that is pronounced enough to be worth treating (the home test's result) or whether you have a problem with severe CSA (if the data from the diagnostic part of the sleep study is to be believed) or some other kind of sleep disordered breathing problem.
It is clear that you have problems with sleep continuity (the arousal data from both the home sleep test and the ASV test, along with the sleep stage hypnographs for the diagnostic part of the split study and the ASV study), but it's also clear that the data indicates that much of the sleep continuity problem is NOT directly associated with sleep disordered breathing. The in-lab tests seem to indicate that PLMs are not an issue, but then again, there's not much sleep in either lab test to go on.
If you do decide to do another sleep test, I'd suggest a plain diagnostic test---a test without a PAP or ASV for the entire night. I would also strongly recommend that you focus on doing what you can to insure that you actually sleep during the study. In other words, if I were you I'd seriously consider NOT exercising on the day of the in-lab test. I'd make doubly sure that I had the good ear plugs. And I'd consider asking the sleep doc for a prescription of ONE Ambien tablet to be taken if you're not able to get to sleep within about 30 minutes or so. I'd also suggest sleeping in your preferred sleeping position when you are at home in your own bed. And when setting the test up, you need to be sure to tell the lab that you have had two very bad sleep test experiences---one because you could hear the tech coughing all night and one because the room was uncomfortably hot at the beginning of the night and then uncomfortably cold at the end of the night. I'd let the lab know beforehand that on your previous in-lab sleep tests you've gotten less than three hours of sleep each time. Some labs are set up where the patient has at least some control over the room temperature. And you may be able to request a room farther down the hall from the tech's station.
As for what I'd look for on a new diagnostic sleep test: I think you want to see at least 3 1/2 or 4 hours of total sleep time during the night; more would be better. And you need look for some consistency between the new sleep test and either the home sleep test or the diagnostic part of the split study. If the new sleep test looks like either of those, then I'd be inclined to say that you know which of those two diagnostic tests is more accurate. If the new sleep test doesn't look like either of those two tests, then you need to look for whether the new sleep test makes more sense than both of those tests. And you need to look at the number of spontaneous arousals and the number of wakes on the new sleep test very closely---if the spontaneous arousals are far more numerous than the SDB events, then you know there's a problem beyond just the SDB.
Whether to have yet another titration test (and on what machine) would really depend on what the new diagnositic study showed in my opinion.
_________________
| Machine: DreamStation BiPAP® Auto Machine |
| Mask: Swift™ FX Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: PR System DreamStation and Humidifier. Max IPAP = 9, Min EPAP=4, Rise time setting = 3, minPS = 3, maxPS=5 |
Re: HELP AGAIN! ASV or APAP?
The RDI is NOT the same as the arousal index. The RDI only includes respiratory related incidents. The arousal index contains all arousals, regardless of the cause. But since the home sleep test uses "surrogate arousal indicators" it is possible that the arousal index on the second page is over stated.musculus wrote: Yeah, now I see where 43 comes from. Note what OP's sleep doctor wrote in the last sentence of the 'sleep study findings' section, totally misleading interpretation.
http://s14.postimg.org/8ba1aes7l/DSC05640.jpg
I guess 43/hr was higher than the true arousal index since heart rate will fluctuate in normal undisturbed sleep, also 43/hr will most likely make OP feel like a zombie during the day and have ZERO energy for exercise.
And then there's also the fact that, as with many sleep study interpretations, the doc focuses (almost) exclusively on SDB and PLMD events. I think part of that tendency on the part of many sleep docs is based on the fact that it can be very difficult to figure out what to do to try to reduce the number of sponatanous arousals and wakes even when it's clear that there are a lot of them.
As an example, I'll offer my own experience: On my last set of sleep studies my own sleep doc admitted that there were too many spontaneous arousals and wakes, but that he had no real idea of what to do to fix them because there's no clear reason why they're happening (hence they're "spontaneous") and because there's no clear cause for the spontaneous arousals/wakes, there's no underlying problem to "fix". The only idea he had was prescription sleeping medication taken every night for two or three months, more attention to sleep hygiene, and trying not to focus too much attention on the wakes and arousals. And he also suggested that it was important that I make sure that my other health issues (migraine headaches, tension headaches, and TMJ issues) are well under control since any one of those things can easily lead to more wakes and arousals. It's been a long haul this winter, but as the number of wakes I remember have gone down, the way I feel has (slowly) improved. Since I routinely turn my machine Off and On when I wake to reset the pressures at their minimum settings, I can see in my data that there are wakes that I don't remember. It's take a long time for me to learn how to do it, but now I do NOT worry about those wakes I don't remember at all, and slowly they are also decreasing in number.
_________________
| Machine: DreamStation BiPAP® Auto Machine |
| Mask: Swift™ FX Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: PR System DreamStation and Humidifier. Max IPAP = 9, Min EPAP=4, Rise time setting = 3, minPS = 3, maxPS=5 |
Re: HELP AGAIN! ASV or APAP?
Thanks once again for the response. I came back from work and will check your posts as soon as I wake up. Or well maybe after I eat and read the newspaper. Good night
_________________
| Mask: Quattro™ FX Full Face CPAP Mask with Headgear |
| Additional Comments: Trying my best to get quality rest. PR System ONE REMstar BiPAP Auto SV Advanced |
System One Respironics Bipap AutoSV Advanced Quattro Fx
Min EPAP: 13.0 CmH20
Min Pressure Support: 3.5
Max EPAP: 25.0
Max Pressure Support: 5.0
Max Pressure: 20.0
Flex Setting: Bi-Flex - 3
Backup Rate:Auto
Humidification Mode:off
Humidifier Setting:c5
Min EPAP: 13.0 CmH20
Min Pressure Support: 3.5
Max EPAP: 25.0
Max Pressure Support: 5.0
Max Pressure: 20.0
Flex Setting: Bi-Flex - 3
Backup Rate:Auto
Humidification Mode:off
Humidifier Setting:c5
Re: HELP AGAIN! ASV or APAP?
andsleepinow wrote:Lol I agree. I recall the sleep technician stating that something needed to be updated when I took the ASV Titration Study.5) The sleep architecture seems pretty lousy on the in-lab tests; but it's not as bad on the home sleep test.
Most adult Americans have lousy sleep hygiene. Can you describe your sleep hygiene?I considered an oral appliance, yes, but I do not want to rule out CPAP/ASV therapy. I believe that I just need to find which machine to use, and under what pressure.6) Recommendations from the sleep studies. While PAP (of some sort) is mentioned on all of the studies' recommendations for treatment, it is NOT the only recommendation. In particular:
- Home sleep study indicates that the SDB is very mild and appears to be positional. It does say that alternatives to PAP such as an oral device are worth considering. Which raises the question: Did you consider an oral appliance or not?
I believe that my sleep hygiene is better than 90% of all people (At least in the US).[*]The ASV study specifically mentions the overall lack of sleep and recommends "Sleep Hygiene Education." Which raises the question: Did anybody ever follow-up and ask you about your sleep hygiene and provide you with some sleep hygiene guidelines?[/list]
On the split study test the tech increased the pressure from 4cm to 5cm well before you managed to fall asleep with the mask. You can see this by looking at the graphs on page 6 of the split study. It looks to me like the tech increased the pressure from 4 to 5cm about 30 minutes after the titration started. You feel asleep for a short bit when the pressure was at 5cm. At 6cm you actually slept for almost an hour before waking up. The wake and restlessness lasted about 30 minutes or so before you fell back asleep for the last few minutes of the sleep test.Personally I think it was the low level of the pressure on the Split Study (A starting pressure of 4.0? Really? I am better off breathing without the machine!) in conjunction with the damn coughs in the beginning of my study that showed the low fractured sleep.It's just that the sleep tests are all over the place and I think you actually need a proper in-lab diagnostic test based on more than 75 minutes of fractured sleep where it's clear that a large part of the problem on that night was getting to a sound sleep state.
You did get into REM on the ASV titration---but the percent time in REM was not much better than the estimated percent REM on the home sleep test.Also the ASV Titration little sleep because of the high pressure and the warm temperature. When I am at home, I do dream. How do I know? Because I remember having them, and on some rare occasions, on days where I have not had exercised I feel more well rested.
And again you mention the connection between exercise and bad sleep. This is something that you need to be open and honest about with the sleep doc (the old one or a new one if you decide to start over.)
I'm not saying you don't need the ASV. I'm saying that there may be MORE to your wakefulness than sleep disordered breathing. If the only underlying cause of your sleep problems was SDB, then the number of spontaneous arousals on the home sleep test and the number of wakes during the diagnostic part of the split study would not be so high. (And yes, I know you want to blame the wakes on the conditions in the lab test, but the very fact that you are such a light sleeper is indicative of a large number of arousals, and the data indicate that many of your arousals are NOT respiratory related.)Yes, but as someone suggested before, that my ASV data shows a pressure support throughout the data and that it may cause my wakefulness.I also think you need to be considering the sleep continuity problems as being caused by other things in addition to the SDB that you happen to have. It's important to understand that the CPAP and ASV treat only the SDB issues: they don't fix bad sleep that is bad for other reasons. And since the data you've posted from your ASV machine seems to indicate that whatever SDB you do have is well controlled by the ASV, it's time to start considering other things that you need to address.
And then there's this: PAP and ASV machines do take some effort to adjust to. And for some people, these machines can trigger additional arousals and wakes simply because there's so much more physical stimuli that we're dealing with. Eventually the brain learns to ignore it all and trust the machine as a "friend" that makes the breathing better. But in the meantime, the pressure changes (with the ASV in particular), the potential for leaks, the noise of your own breathing, the sensation of air being blown down your throat, and the simple sensation of the mask on your face can all cause short term disruption to your sleep. But dial wingin' doesn't usually fix these problems; time does. And in fact, once the data shows that the AHI is low enough and the leaks are under control, dial wingin' can perpetuate adjustment problems because it takes time to get used to each and every change in settings.
Memory is not as reliable as we want to think it is. You want the log to be easy to keep. All you need to do is design a spreadsheet or even a paper form to fill in. Ideally it should take you less than 10 minutes to fill in the log.While this requires effort, I will do. But I can also act on memory because I usually sleep near the same time and it usually does not take long for me to fall asleep. 10-15 minutes most nights.A sleep log is one thing that might be useful. Track when you go to bed, when you get up, and estimates of how long you think it took you to fall asleep, how many times you woke up during the night, and how long you think you actually slept during the night. Since you think that exercise makes the sleep worse, you need to track that as well as how you (subjectively) about the sleep each morning.
I'd suggest designing a spreadsheet or paper form to fill in that lets you quickly write down the following information at the end of each day just before you go to bed:
- What kind of exercise did you do?
- When did you exercise?
- How long did you exercise?
- Relatively speaking, how intensely did you exercise for you?
- What time did you go to bed?
- How long did it take you to fall asleep? (Estimate this----do NOT look at a clock)
- Do you remember any wakes or restlessness? If so, how many wakes or restless periods?
- When did you wake up for the morning? When did you get out of bed?
- Estimate how much sleep you go during the whole night.
- How rested do you feel on waking?
- Do you remember dreaming? (This is optional)
_________________
| Machine: DreamStation BiPAP® Auto Machine |
| Mask: Swift™ FX Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: PR System DreamStation and Humidifier. Max IPAP = 9, Min EPAP=4, Rise time setting = 3, minPS = 3, maxPS=5 |
Re: HELP AGAIN! ASV or APAP?
Out of curiosity, does your AHI go up or stay the same on the night after exercising? Or is it just that the sleep deteriorates because the number of wakes goes up and the restlessness goes up?The differences I can draw from exercising vs not exercising is that I wake up many more times when I exercise and notice/wake up from my dreams much more.
And when you wake up from the dreams, are you waking up from bad dreams? Is there any chance that nightmares or night terrors are potential sleep problems for you? (Night terrors is a NREM sleep disorder)
When you say you "breathe harder" during the days after an exercise day, do you mean that you are panting and short of breath? Do you mean you are breathing more rapidly than on the exercise day? And does this happen during the DAYS after the exercise day as well as at night(s)? If there is a DAYTIME breathing problem on the day(s) following an exercise day, then you need to be examined for DAYTIME breathing problems such as asthma. (There is one version of asthma that can be triggered by too much exercise in fact.) And if there is a DAYTIME breathing problem on the day after you exercise, you need to bring this up with your primary care physician. You may need a referral to pulmonologist to investigate the DAYTIME breathing problem if exercise is affecting your DAYTIME breathing on the day after you exercise.Usually exercising one day requires for me not to exercise about three days consecutively for me to feel well rested. I have experimented myself in this situation many times and it indeed is true. I definitely also breathe harder during these three days
I'll be honest, I'm not following all of this. When you say you are "breathing too strong for the weak 5.5 EPAP pressure", you've lost me. The EPAP pressure only needs to be high enough to prevent your airway from collapsing in an OA. Higher EPAP pressures make it harder to exhale against the pressure, and that makes it harder to breath (when you are awake at least) rather than easier to breathe.I definitely also breathe harder during these three days which might mean that I need a higher pressure from my machines because my breathing is too strong for the weak 5.5 EPAP pressure that I have.
The CSA problem that ASV's are designed to fix is more accurately described as "not breathing strongly enough" to blow off enough CO2: Essentially CSA is caused by an undershoot/overshoot cycle in the CO2 levels. The cycle starts when the brain has trouble interpreting the CO2 levels and "forgets" to send a signal to breath deeply enough and the breath becomes shallower and shallower and not enough CO2 is exhaled (the undershoot part of the cycle); eventually the brain forgets to send a signal to inhale for a long enough time for a Central Apnea to be scored. And while the breathing is becoming shallower and shallower, the CO2 levels are growing because you're not exhaling enough CO2 during the exhalations. Eventually (after the CA), the brain realizes that it needs to restart the breathing, typically because of the drop in O2 connected with the CA. But at this point the brain also notices that the CO2 levels are too high and so it sends a signals to breath very deeply, which blows off too much CO2 (the overshoot part of the cycle) and then the cycle starts over: As the CO2 level goes too low, the brain starts forgetting to send a signal to breath deeply enough and the breaths start to become shallower and shallower again.
It's this undershoot/overshoot cycle on the CO2 levels that an ASV is designed to fix and the way an ASV fixes this undershoot/overshoot cycle is that it monitors the depths of the inhalations. When the the depth of the inhalations fails to meet the target ventilation, the ASV rapidly and drastically increases the IPAP pressure to "trigger" an inhalation and insure that enough air is inhaled to insure proper gas exhange in the lungs, which stabilizes the CO2 levels and prevents the undershoot/overshoot cycle from getting started in the first place. But those drastic increases in IPAP do take some getting used to, and until you do, they can be a source of additional wakes and arousals.
_________________
| Machine: DreamStation BiPAP® Auto Machine |
| Mask: Swift™ FX Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: PR System DreamStation and Humidifier. Max IPAP = 9, Min EPAP=4, Rise time setting = 3, minPS = 3, maxPS=5 |
Re: HELP AGAIN! ASV or APAP?
You still haven't answered my question. What time of day do you exercise?I exercise on very good times. I have done my research of many things related to exercise and read a great book on the science part of it. I definitely do not do intense exercise anymore, but even a little will disrupt my sleep.It could be that you need to pay careful attention to when you exercise. For many people exercising too close to bedtime will make it more difficult to get to sleep and stay asleep. You might also find that too much intense exercise on one particular day is problematic, so you may need to cut back on how much exercise you do at any given time, but increase the number of days per week that you do something.
Good.I had Zero caffeine (No chocolate, coffee, soda, tea, etc.) for over two yearsAlso look at things like caffeine consumption. We tend to consume more caffeine than we realize and we tend to drink it later in the day than we think---particularly when we're feeling excessively sleepy or tired during the day.
Now: What about alcohol? What about sugar? What about carbs? All of these things too close to bed can also adversely affect sleep.
And are you on any daily medication for other medical problems?
Vitamin D levels are low in lots of people regardless of diet. Scheduling a good thorough physical after you are done with your semester is a very good idea. Be sure to mention all the problems with exercise at that physical too.I eat very healthy food so my vitamins are definitely good. Better than many people. As for thyroid, I will get that checked too along with a physical exam. But that would have to be after school semester ends in May.And finally, it's worth considering other causes of the daytime sleepiness and fatigue. If it's been a while since you've had a full physical exam, it's time to set one up and have all the usual (non-SDB) suspects for daytime fatigue investigated: Get your thyroid checked and your vitamin levels checked in particular.
Technically your ASV study meets all the standards for an "optimal" titration except for the fact that the 19 minutes of REM sleep was NOT supine REM sleep. (See http://www.aastweb.org/Resources/Guidel ... mmary.pdf) But you don't believe the settings that came out of that study are "proper". Unfortunately self-titrating an ASV by dial wingin' is a whole lot harder than trying to self-titrate an APAP or CPAP; there are a whole lot more therapeutic settings that have to be set and the data you've posted doesn't really indicate that anything is obviously "wrong" with your settings. In other words, the main problem seems to be that you just are not yet feeling as well as you should be feeling and your sleep is still bad in terms of the number of unwelcome wakes and in terms of not feeling rested when you wake up.In conclusion, I still do think that I need to know what proper settings and machine to use because the ASV has helped me a lot.
If central apneas are a problem, then a higher than needed CPAP pressure can trigger additional CAs. On the ASV side if the settings are not correct it can aggravate the CSA problem rather than fix it.This raises a question that I have. What is the downside of having a slightly higher CPAP or ASV setting than is needed? Will it cause harm? If so, how and why?
For someone who doesn't have problems with pressure induced central apneas, the biggest problem with too much pressure is that too much pressure can lead to additional adjustment problems, such as more problems with leaks, dry mouth, aerophagia, and overall discomfort. And all of these additional problems can and do lead to more spontaneous arousals, which in turn can lead to additional sleep problems.
I'm not a doctor or a sleep tech. I'm just a well read OSA patient who uses a plain old BiPAP Auto.And by the results of these tests, there is no way to tell what machine I should be using under which pressure?
Keeping that in mind, I think that the ASV and CPAP titrations are both problematic mainly because you don't have an accurate diagnosis. The CPAP titration also has no REM sleep and the ASV titration has no supine REM sleep.
If the home sleep study is correct, then CPAP/APAP ought to be fine and the CPAP titration part of the split study indicates that a pressure of 6 should be a sufficient starting point. And if wanted to dial wing with the APAP it would be reasonable to set the APAP up in Auto mode with a range of 6-8 or 6-10 if you wanted to see if the machine wanted to increase the pressure. (If you're not comfortable breathing at 6 cm, you could up the starting pressure to 7cm without too much risk of causing additional problems.)
If the data in diagnostic part of the split study is correct, then an ASV machine is probably more appropriate and the ASV titration says that the settings that came out of that test are appropriate. And if those are the settings you are currently using on the ASV, I don't think I'd mess with them.
If the CAs in the diagnostic part of the split study should have been scored as OAs (and there is no way for us to determine that), then the CPAP titration part of that study indicates that CPAP at 6cm should be suficient, but again since there was no REM sleep, it might be reasonable to set the APAP up in a narrow auto mode of 6-8 or 6-10 cm.
As for which is the right thing to do? I'd say you need to talk to a sleep doc who's seen the data. If that cannot happen until your semester is over, you're stuck with what makes you feel the best? You've said that its the ASV machine. It may be that you simply need to give it more time since learning to sleep with an ASV is not easy.
And it's now almost 20 minutes after my "official bedtime" of 1:30AM and I'm starting to yawn. Which means it's time for me to go to bed. I probably won't read anything here tomorrow because I've got a long day at work.
_________________
| Machine: DreamStation BiPAP® Auto Machine |
| Mask: Swift™ FX Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: PR System DreamStation and Humidifier. Max IPAP = 9, Min EPAP=4, Rise time setting = 3, minPS = 3, maxPS=5 |
Last edited by robysue on Wed Apr 16, 2014 6:47 am, edited 1 time in total.
Re: HELP AGAIN! ASV or APAP?
Who recommended that?sleepinow wrote:It was more of a recommendation from forum users on here.robysue wrote:2) It's not at all clear why the doc agreed to an ASV titration.
You Kids Have Fun!!
Re: HELP AGAIN! ASV or APAP?
Forgot to mention this before: There were NO (as in ZERO) apneas of any kind scored during the entire ASV test.sleepinow wrote:How can you tell? Because I can't. I could have sworn though that the pressure was low in the beginning and increased in time to counter the apneas I was having. (emphasis added)On the ASV titration study it is not clear how the settings were arrived at. It appears that the tech started you out with the settings that wound up being the recommended pressure settings
So whatever the things you are remembering as "the apneas I was having" actually are, they are NOT apneas that can be scored on an in-lab sleep test.
_________________
| Machine: DreamStation BiPAP® Auto Machine |
| Mask: Swift™ FX Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: PR System DreamStation and Humidifier. Max IPAP = 9, Min EPAP=4, Rise time setting = 3, minPS = 3, maxPS=5 |
Re: HELP AGAIN! ASV or APAP?
I find this to be true. At home, I have turned my room into a great place to sleep because I nearly removed everything that would wake me up (except for my very old aunt who at times likes to scream).musculus wrote:Since you cannot sleep very well in labs (you seems to be a very light sleeper
I have copied and pasted your suggestions into a word document, and I will print it out to use the information for whatever decisions I need to make.
Edit: I will read everyones posts and respond to it with individual posts. It will take some time but I will finish reading everyone's post
_________________
| Mask: Quattro™ FX Full Face CPAP Mask with Headgear |
| Additional Comments: Trying my best to get quality rest. PR System ONE REMstar BiPAP Auto SV Advanced |
System One Respironics Bipap AutoSV Advanced Quattro Fx
Min EPAP: 13.0 CmH20
Min Pressure Support: 3.5
Max EPAP: 25.0
Max Pressure Support: 5.0
Max Pressure: 20.0
Flex Setting: Bi-Flex - 3
Backup Rate:Auto
Humidification Mode:off
Humidifier Setting:c5
Min EPAP: 13.0 CmH20
Min Pressure Support: 3.5
Max EPAP: 25.0
Max Pressure Support: 5.0
Max Pressure: 20.0
Flex Setting: Bi-Flex - 3
Backup Rate:Auto
Humidification Mode:off
Humidifier Setting:c5
Re: HELP AGAIN! ASV or APAP?
My doctor did not even receive the raw data. He just was following the same data that I have posted here with the ASV Titration summary reports. I have the same feeling he would have received the summary too for the split study. I will ask the sleep center if I can have the raw data. Is it illegal not to give full information to the patient? I read a law somewhere that the patient is now allowed to receive study results.robysue wrote: If the tech had reason to change the settings, there would be one line for each set of settings that were tried. Thanks for looking into it. I felt like that is how sleep technicians worked; starting with the lowest pressure and working their way up. That is a big reason why I thought he might have started at a different pressure and also the fact that it felt like the pressure was low during commencement.
True.Perhaps someone with ASV experience can say something about how the initial settings on an ASV titration are arrived at.
Alright that makes more sense. I originally thought that their software was outdated because it felt odd to me that the ASV Titration did not include too much information e.g AHII really don't know how scoring is done, but I was under the impression that the initial scoring of a sleep test is often checked for accuracy after the test is done by going back through the data carefully.
I copied some of the useful information below, it looks like this summer is going to be one hell of a summer :/
(Note that when I asked for my raw data on my sleep studies I got no where; the doc's office was simply unwilling to provide it to me in any form whatsoever.)
_________________
| Mask: Quattro™ FX Full Face CPAP Mask with Headgear |
| Additional Comments: Trying my best to get quality rest. PR System ONE REMstar BiPAP Auto SV Advanced |
System One Respironics Bipap AutoSV Advanced Quattro Fx
Min EPAP: 13.0 CmH20
Min Pressure Support: 3.5
Max EPAP: 25.0
Max Pressure Support: 5.0
Max Pressure: 20.0
Flex Setting: Bi-Flex - 3
Backup Rate:Auto
Humidification Mode:off
Humidifier Setting:c5
Min EPAP: 13.0 CmH20
Min Pressure Support: 3.5
Max EPAP: 25.0
Max Pressure Support: 5.0
Max Pressure: 20.0
Flex Setting: Bi-Flex - 3
Backup Rate:Auto
Humidification Mode:off
Humidifier Setting:c5
Re: HELP AGAIN! ASV or APAP?
robysue wrote:Second page of the Home Sleep Study report clearly lists the AROUSALS/HOUR as 43. See the red rectangle in the (edited) version of sleepinow's Home Sleep Study report:musculus wrote: Also, I don't know why people say you got arousal index of 43 (that's very poor sleep), all I could see is 43 BPM event with index of 6 in your home study.
The red rectangle is at the FAR RIGHT of the page by the Pulse Rate with Arousals Indicators graph. That's why sludge and I have pointed out that there are a lot of (non respiratory related) arousals on this home sleep test.
That said, it's true that the home sleep doesn't have an EEG channel. They're using other data to infer when the arousals happened and whether the suspected arousals are related to sleep disordered breathing.
Wow this is information that I have missed. I did not even notice that. It is a little mind blowing now that you have shown that information. My doctor did not even mention of this when visited him for a check up and he went over the results of the home sleep study
_________________
| Mask: Quattro™ FX Full Face CPAP Mask with Headgear |
| Additional Comments: Trying my best to get quality rest. PR System ONE REMstar BiPAP Auto SV Advanced |
System One Respironics Bipap AutoSV Advanced Quattro Fx
Min EPAP: 13.0 CmH20
Min Pressure Support: 3.5
Max EPAP: 25.0
Max Pressure Support: 5.0
Max Pressure: 20.0
Flex Setting: Bi-Flex - 3
Backup Rate:Auto
Humidification Mode:off
Humidifier Setting:c5
Min EPAP: 13.0 CmH20
Min Pressure Support: 3.5
Max EPAP: 25.0
Max Pressure Support: 5.0
Max Pressure: 20.0
Flex Setting: Bi-Flex - 3
Backup Rate:Auto
Humidification Mode:off
Humidifier Setting:c5
Re: HELP AGAIN! ASV or APAP?
I do not know what was misinterpreted I apologizemusculus wrote:Yeah, now I see where 43 comes from. Note what OP's sleep doctor wrote in the last sentence of the 'sleep study findings' section, totally misleading interpretation.
http://s14.postimg.org/8ba1aes7l/DSC05640.jpg
I guess 43/hr was higher than the true arousal index since heart rate will fluctuate in normal undisturbed sleep, also 43/hr will most likely make OP feel like a zombie during the day and have ZERO energy for exercise.
_________________
| Mask: Quattro™ FX Full Face CPAP Mask with Headgear |
| Additional Comments: Trying my best to get quality rest. PR System ONE REMstar BiPAP Auto SV Advanced |
System One Respironics Bipap AutoSV Advanced Quattro Fx
Min EPAP: 13.0 CmH20
Min Pressure Support: 3.5
Max EPAP: 25.0
Max Pressure Support: 5.0
Max Pressure: 20.0
Flex Setting: Bi-Flex - 3
Backup Rate:Auto
Humidification Mode:off
Humidifier Setting:c5
Min EPAP: 13.0 CmH20
Min Pressure Support: 3.5
Max EPAP: 25.0
Max Pressure Support: 5.0
Max Pressure: 20.0
Flex Setting: Bi-Flex - 3
Backup Rate:Auto
Humidification Mode:off
Humidifier Setting:c5
Re: HELP AGAIN! ASV or APAP?
But it is odd that the number of spontaneous arousals---those that are NOT associated with respiratory problems---is so much greater on the in home sleep test than it is on the in-lab sleep tests. And the thing is, if you typically have this many arousals in your own bed, that could explain the continuing problems with daytime functioning. And so the question becomes, "How do you minimize the spontaneous arousals?" And I don't have an answer to that question.
Ouch.
Is it quite possible that the CPAP got rid of the awakenings? And is it also possible that the sleep technician did not include spontaneous arousals for whatever reason it may be?Even so: On the ASV titration, there were 25 awakenings and 24 spontaneous arousals in spite of the ASV treatment. On the split test, there were NO spontaneous arousals on either part of the night, but there were 24 awakenings, most of which occurred during the diagnostic part of the night. So while the spontaneous arousal index on the in-lab tests may be less than the home sleep test, there's still an obvious problem with sleep continuity that doesn't seem to be associated with SDB.
True. I was better able to deal with the cold. Anyways being sweaty is common when sleeping and I researched that it is also commonly associated with sleep apnea. This might ring to because when falling asleep, it was not hot for me, but later on during the night my body temperature probably rose and I started feeling uncomfortable. If I had not had any disturbed sleep, the warmth feeling might of not affected me in such a way. I have similar experiences of that at home but I keep it nice and cold to prevent myself from being too disturbed by any hot feelingSo you had two exceptionally bad nights in the lab as far as getting and staying asleep are concerned. That means that it's really hard to get a sense of what's really going on with your sleep with or without the PAP. Which means that you still don't have a really good idea of just what's going on in your sleep, and hence you don't really know what (if anything) PAP can really do for you---regardless of whether its CPAP or an ASV machine.
Yes, Yes, and I did not know they were more difficult. The wires and someone watching me did not enter my mind as troubling. I actually felt comfortable with that, but with the doctor coughing and my crappy earplugs, that probably took off about an hour of sleep I possibly would have had.So correct me if I'm wrong: You know you don't sleep well when you exercise, and so you exercised (a bit more than usual) before the in-lab sleep tests, which are known to be difficult because you're asked to sleep in a strange place with wires all over you and someone watching you all night long?
Son of aQuite frankly it's a bit of a surprise to me that with only 75 minutes of sleep time during the diagnostic part of the sleep study that they bothered to wake you up and put a mask on you. Typically labs insist on at least 120 minutes of sleep during the diagnostic part of a split study to move onto the titration part of the test.
It's not clear if you have a sleep disordered breathing problem that is pronounced enough to be worth treating (the home test's result) or whether you have a problem with severe CSA (if the data from the diagnostic part of the sleep study is to be believed) or some other kind of sleep disordered breathing problem.
I rewrote these /\ \/ twice to respond to it and make it easier to read (at least that is my intention)
The ASV did very significantly help me not be tired. So in my opinion I think it is worth treating. I was on the verge of quitting school because of my tiredness and anticipated leaving my job because I was too tired. The ASV has saved me from doing that. But is an ASV what I need? Who knows?It's not clear if you have a sleep disordered breathing problem that is pronounced enough to be worth treating
Isn't CSA and sleep disordered breathing completely related to each other?(if the data from the diagnostic part of the sleep study is to be believed) or some other kind of sleep disordered breathing problem. [/quote](the home test's result) or whether you have a problem with severe CSA
It is extremely rare that I sleep without waking up at least once. I think I woke up once yesterday's night, but before that it was probably two years ago when I was running a lot.It is clear that you have problems with sleep continuity (the arousal data from both the home sleep test and the ASV test, along with the sleep stage hypnographs for the diagnostic part of the split study and the ASV study), but it's also clear that the data indicates that much of the sleep continuity problem is NOT directly associated with sleep disordered breathing.
The reason why I did it is because someone mentioned that I should be at my worst by exercising to get a pressure that I would need that would help me more when I do exercise since I plan on doing it once I treat whatever is wrong with me. It made sense at the time to do it, but we were not fully aware that I did not sleep much at all.If you do decide to do another sleep test, I'd suggest a plain diagnostic test---a test without a PAP or ASV for the entire night. I would also strongly recommend that you focus on doing what you can to insure that you actually sleep during the study. In other words, if I were you I'd seriously consider NOT exercising on the day of the in-lab test.
I'd make doubly sure that I had the good ear plugs. And I'd consider asking the sleep doc for a prescription of ONE Ambien tablet to be taken if you're not able to get to sleep within about 30 minutes or so.
My preferred sleeping position is on my back, but sleeping on my back worsens my therapy to a big extent.I'd also suggest sleeping in your preferred sleeping position when you are at home in your own bed.
And when setting the test up, you need to be sure to tell the lab that you have had two very bad sleep test experiences---one because you could hear the tech coughing all night and one because the room was uncomfortably hot at the beginning of the night and then uncomfortably cold at the end of the night. I'd let the lab know beforehand that on your previous in-lab sleep tests you've gotten less than three hours of sleep each time. Some labs are set up where the patient has at least some control over the room temperature. And you may be able to request a room farther down the hall from the tech's station.
Got it. I copied most of these helpful recommendations in a word document
I came here thinking that a sleep study would diagnose what is wrong with me. So far it has just slightly given me a better idea of what could possibly be wrong, yet I am still very much bewildered.As for what I'd look for on a new diagnostic sleep test: I think you want to see at least 3 1/2 or 4 hours of total sleep time during the night; more would be better. And you need look for some consistency between the new sleep test and either the home sleep test or the diagnostic part of the split study. If the new sleep test looks like either of those, then I'd be inclined to say that you know which of those two diagnostic tests is more accurate. If the new sleep test doesn't look like either of those two tests, then you need to look for whether the new sleep test makes more sense than both of those tests. And you need to look at the number of spontaneous arousals and the number of wakes on the new sleep test very closely---if the spontaneous arousals are far more numerous than the SDB events, then you know there's a problem beyond just the SDB.
Whether to have yet another titration test (and on what machine) would really depend on what the new diagnositic study showed in my opinion.
_________________
| Mask: Quattro™ FX Full Face CPAP Mask with Headgear |
| Additional Comments: Trying my best to get quality rest. PR System ONE REMstar BiPAP Auto SV Advanced |
System One Respironics Bipap AutoSV Advanced Quattro Fx
Min EPAP: 13.0 CmH20
Min Pressure Support: 3.5
Max EPAP: 25.0
Max Pressure Support: 5.0
Max Pressure: 20.0
Flex Setting: Bi-Flex - 3
Backup Rate:Auto
Humidification Mode:off
Humidifier Setting:c5
Min EPAP: 13.0 CmH20
Min Pressure Support: 3.5
Max EPAP: 25.0
Max Pressure Support: 5.0
Max Pressure: 20.0
Flex Setting: Bi-Flex - 3
Backup Rate:Auto
Humidification Mode:off
Humidifier Setting:c5