I want to THANK many of you who have helped me on my journey to successful ASV therapy. Those of you who so generously shared your time and advice will immediately know who you are. Those of you who frequent this forum can probably guess. I owe each of you a great deal of gratitude!Oops! This started out to be a brief account of my journey to ASV, but turned into a tome. Welcome, if you've joined, but feel free to drop off at any turn in the road.
First an important caveat: I am NOT suggesting than anyone read this and decide to venture into this degree of self-directed therapy. I did it with a LOT of research and I was VERY CONSERVATIVE in my approach. My motive was simple: Neither the doc nor the DME were concerned with my therapy. That became abundantly clear from day ONE. It was my problem to deal with and resolve!
I am writing this post . . .
1. Primarily for those newbies who are going through general frustrations.
2. More specifically, for those of you who are struggling with your doc and/or DME and feeling frustrated because your therapy is not going as you want/need.
3. Finally, to give some Medicare information that might be beneficial.
I began CPAP therapy in November 2011. Based upon two sleep studies, the doc started me on a ResMed S9 Elite @ 10cm h2o. From day one, the straight CPAP did not work for me. I had a follow-up visit with my doc. I explained my concern over CAs, but he didn’t seem the least concerned. I talked with my DME about potentially changing machines and she indicated Medicare would NOT authorize a CPAP replacement. She said, “for Medicare to approve a change, I would have to have a treated AHI of over 14.0 and the majority of them CAs.”
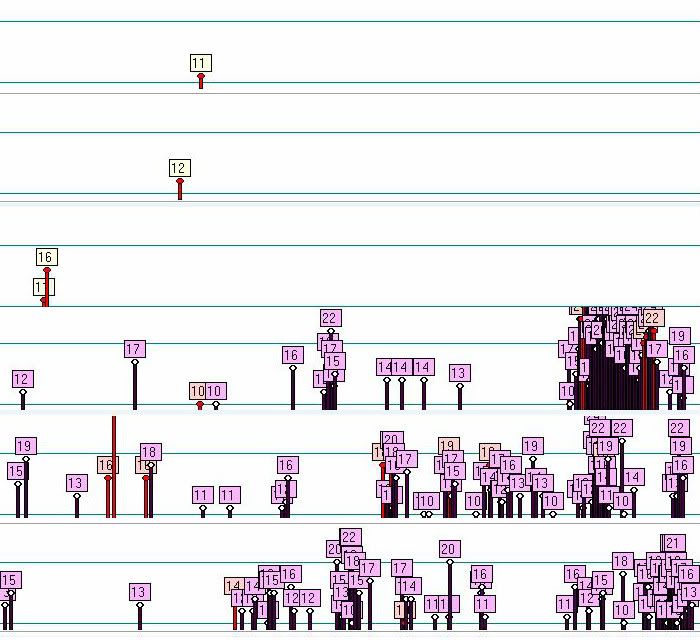
Feeling a total lack of support, I decided to take my therapy into my own hands. I located and purchased a used ResMed VPAP SV on craigslist. I literally guessed at pressure settings of EEP = 6, Min PS = 3 and Max PS = 8. On the first night I had zero apneas. So I started accumulating data. I was having so few events that I began to question if the VPAP was scoring events properly. So (yes it’s true) a bought a second VPAP and also a Respironics BiPAP autoSV. I got some very valuable advice from several cpaptalk members regarding the pressure settings for the BiPAP machine. I had the same favorable results with all three machines. Here are the numbers for straight CPAP and VPAP/BiPAP:
CPAP: 60 days: CA: 6.1, AI: 7.1, HI: .06, AHI: 7.7
VPAP/BiPAP: 30 days: AI: 0.1, HI: 1.7, AHI: 1.8
I put together a pile of graphs and charts and had another appointment with my doc. I went through the data and he asked, “Where did you get these data?” I told him that I downloaded them from the Elite, VPAP and BiPAP machines.
With multiple charts and graphs showing 0 – 2 apneas per night versus 50 – 60 per night, it was hard to debate the success of the ASV therapy over the CPAP therapy.
After looking perplexed he said, “I can’t use that data.” My response was that I was neither asking nor expecting him to. My motive was simple, to point out to him that I was not satisfied with my therapy and I expected him to do another sleep study and determine if I needed ASV therapy. I wasn’t going to allow him to miss the fact that I was able to attain a better result on my own than I had gotten from him. Without sounding like a threat, I informed him that I would prefer my therapy to be under his supervision and, of course, covered by Medicare, but if he couldn’t justify the sleep study, I would just continue to manage my own therapy.
He scheduled an ASV sleep study for 2-29-12. On 3-16-12, I picked up my prescription for a PR System One BiPAP autoSV.
So the journey to ASV ends and, the one-night-at-a-time, life-time of ASV therapy begins . . .
My DME experience was flawed and fatal from the beginning. They leased me (Medicare) a used machine. When I realized it was used, I questioned her. First she said it was new, but when I indicated I knew the Hours of Use, she indicated that Medicare required NEITHER a new nor even current model. (I still don’t know if that is true or not.) Multiple calls and contacts with her resulted in misleading and often totally inaccurate information. I was preparing to write a letter to the owner/manager, when I made a recent phone call to her and was informed, “that she is no longer with the company.” Apparently others made it to management before me.DME Issues:
As indicated above, my DME totally misinformed me regarding the Medicare requirement. In order to qualify for this transition from straight CPAP my doc only had to answer YES to these specific Yes/No questions:Medicare Issue:
RAD Qualifications: (for BiPAP autoSV mode)
1. Has patient failed CPAP therapy?
2. Is AHI > 5?
3. Is % of central apneas > 50% of total?
4. Are central apneas / hypopneas >= 5/ hour?
5. Diagnosis of CSA or CompSA?
So, even though I am still within the 13 month “lease” period for the S9 Elite, I am able to transition to the ASV therapy.
PHILOSOPHICALLY: One of the things that has concerned me most about many newbies’ postings on this forum is the suggestion that they are about to give up and discontinue therapy. In a previous post I mentioned something that I had read – CPAP therapy and marriage have about the same “divorce” rate. Each has about a 50% chance of failure. Success should be your only objective. It’s too critical to your health and too important to your family!Newbie issues:
It’s no surprise to any of you that xPAP therapy is a challenge. You wouldn’t be reading this unless you were benefiting from the information on cpaptalk. What you hear over and over is to take each challenge separately and, as with AA, one night at a time. I, as all the frequent posters, went through the same trials and travails. Looking back, sometime I think just the options for changes in therapy sort of made it a “game” and took some of the frustration out of it. If you haven’t yet, within a few months, you will probably have a drawer full of discarded failed mask attempts, your bed decked out with your hose hanger and hose cozy, cpap pillow, your pad-a-cheek or T-shirt liners (or both), gecko nose pads, etc., etc. But keep in mind, as you go through the issues that things do get better. As impossible as it may seem when you are fighting your way through, that some night (after 10 days, 50 days or 100 days) you will realize that you do not even feel the mask on your face and you can’t tell if there is even any pressure. You will reach up to the vent holes to see if air is escaping! Most importantly, one morning you will wake up and feel better than you probably have in years. Additionally your partner will probably be reacquainted with a much less grouchy person.
Always keep in mind that there is a wealth of knowledge and experience among cpaptalk members and they are very generous with their time. So come back often with questions and learn what you need to succeed”
PRACTICALLY: With my opening caveat in mind, you (and your family) is/are the one/s most concerned with your success in xPAP therapy. Yes, as mentioned above, there are many here willing and able to help, but in the final analysis, you have to drive your own therapy. Almost unanimously, posters feel their docs and DMEs offer little help and support – clearly I agree. That is specifically why I took the therapy into my own hands. You’re lucky enough to be on the forum. If you’re lucky enough to have a supportive doc and/or DME then life is better. But regardless, for your health and the well-being of your family, it is important for you to stick with the therapy, meet and defeat the challenges, work with (fight, if necessary) your doc and/or DME and gain the benefits of successful therapy.
Here's to your successful therapy and serene sleep! I hope your journey won't be as bumpy as mine, but just as fulfilling!












