Build Home Sleep Lab < $1000
- Jay Aitchsee
- Posts: 2936
- Joined: Sun May 22, 2011 12:47 pm
- Location: Southwest Florida
Re: Home Sleep Lab < $1000
Wow Liz, that's way cool. Good job on getting the 30 sec data down already.
I'm not going to try to analyze your charts, way to foggy for that, but they sure look good. Funny, how you started out in REM?
Jay
I'm not going to try to analyze your charts, way to foggy for that, but they sure look good. Funny, how you started out in REM?
Jay
_________________
| Mask: AirFit™ P10 Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: S9 Auto, P10 mask, P=7.0, EPR3, ResScan 5.3, SleepyHead V1.B2, Windows 10, ZEO, CMS50F, Infrared Video |
- Lizistired
- Posts: 2835
- Joined: Tue Dec 14, 2010 10:47 pm
- Location: Indiana
Re: Home Sleep Lab < $1000
It's indicated REM all three nights when I first put it on and may not even be in bed yet. Must be similar waves when I'm getting hooked up. All the other data seems pretty accurate though.
_________________
| Mask: Swift™ LT Nasal Pillow CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Swift FX sometimes, CMS-50F, Cervical collar sometimes, White noise, Zeo... I'm not well, but I'm better. |
ResScan: http://www.resmed.com/int/assets/html/s ... c=patients
ResScan Tutorial- http://montfordhouse.com/cpap/resscan_tutorial/
Machines Video: http://www.cpaplibrary.com/machine-education
ResScan Tutorial- http://montfordhouse.com/cpap/resscan_tutorial/
Machines Video: http://www.cpaplibrary.com/machine-education
- Jay Aitchsee
- Posts: 2936
- Joined: Sun May 22, 2011 12:47 pm
- Location: Southwest Florida
Re: Home Sleep Lab < $1000
As well you should. Look at all that deep sleep!Lizistired wrote:...I actually feel pretty decent this morning...
j
_________________
| Mask: AirFit™ P10 Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: S9 Auto, P10 mask, P=7.0, EPR3, ResScan 5.3, SleepyHead V1.B2, Windows 10, ZEO, CMS50F, Infrared Video |
- Jay Aitchsee
- Posts: 2936
- Joined: Sun May 22, 2011 12:47 pm
- Location: Southwest Florida
Re: Home Sleep Lab < $1000
_________________
| Mask: AirFit™ P10 Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: S9 Auto, P10 mask, P=7.0, EPR3, ResScan 5.3, SleepyHead V1.B2, Windows 10, ZEO, CMS50F, Infrared Video |
- Lizistired
- Posts: 2835
- Joined: Tue Dec 14, 2010 10:47 pm
- Location: Indiana
Re: Home Sleep Lab < $1000
JeffH posted this in another thread...Jay Aitchsee wrote:Check out this Dr's home sleep lab!
http://quantdoctor.com/2011/09/17/the-q ... ightstand/
J
http://news.cnet.com/8301-27083_3-20112 ... e+Atlas%29
I was hoping ZEO would go toward the environment tracking that was in your link. It would be interesting to see noise, temp changes, maybe light overlayed with the sleep results.
How long do you go before replacing your sensor? Or have you yet. I think their site says 90 days, yeah, right.
I got good data for the first half of last night, But this morning the sensor shifted and I think the room got a little warm and I imagine sweat interfers with it.
_________________
| Mask: Swift™ LT Nasal Pillow CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Swift FX sometimes, CMS-50F, Cervical collar sometimes, White noise, Zeo... I'm not well, but I'm better. |
ResScan: http://www.resmed.com/int/assets/html/s ... c=patients
ResScan Tutorial- http://montfordhouse.com/cpap/resscan_tutorial/
Machines Video: http://www.cpaplibrary.com/machine-education
ResScan Tutorial- http://montfordhouse.com/cpap/resscan_tutorial/
Machines Video: http://www.cpaplibrary.com/machine-education
- Jay Aitchsee
- Posts: 2936
- Joined: Sun May 22, 2011 12:47 pm
- Location: Southwest Florida
Re: Home Sleep Lab < $1000
I wore mine first on June 25th. Somehow, it seems longer than two months. I don't have any trouble when I wear mine attached to the Quattro FFM headgear. If I wear it with the Zeo band when I'm using Nasal Pillows (rare), the band sometimes rides up the back of my head and gets loose and drops the signal. Occaisionally, even with the quattro headgear, it will drop the signal for five to ten minutes during the night. I don't know if it looses the signal, or it just can't figure out what's going on. It doesn't happen often enough for me to worry about it and I haven't really looked at the video to see. I do know that it is pretty sensitive to movement and if you touch it, or fool around with it, the dislplay drops the little "mickey mouse" status symbol. I do wipe the sensors gently with a cpap wipe each evening as I do my mask and face. Since it's woolite washable, I figure a gentle wipe won't hurt it.
Yeah, I don't know about the 90 day thing. My guess is that it should be good for at least 180.
I don't know if I can handle many more sensors. I'm spending an at least hour every morning now collating and fooling with this data.
So, are you planing on taking advantage of some of the coaching? I think they want you to have at least 7 nights data before starting. I don't know if you've had a chance yet, but there's a lot of good info in the Blog/forum/customer service areas. Not the easiest to root out though, kind of like this forum.
OK, enough rambling. Later,
J
Yeah, I don't know about the 90 day thing. My guess is that it should be good for at least 180.
I don't know if I can handle many more sensors. I'm spending an at least hour every morning now collating and fooling with this data.
So, are you planing on taking advantage of some of the coaching? I think they want you to have at least 7 nights data before starting. I don't know if you've had a chance yet, but there's a lot of good info in the Blog/forum/customer service areas. Not the easiest to root out though, kind of like this forum.
OK, enough rambling. Later,
J
_________________
| Mask: AirFit™ P10 Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: S9 Auto, P10 mask, P=7.0, EPR3, ResScan 5.3, SleepyHead V1.B2, Windows 10, ZEO, CMS50F, Infrared Video |
- Jay Aitchsee
- Posts: 2936
- Joined: Sun May 22, 2011 12:47 pm
- Location: Southwest Florida
Re: Home Sleep Lab < $1000
I see the price of the Zeo bedside unit officially dropped to $149 today.
Jay
Jay
_________________
| Mask: AirFit™ P10 Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: S9 Auto, P10 mask, P=7.0, EPR3, ResScan 5.3, SleepyHead V1.B2, Windows 10, ZEO, CMS50F, Infrared Video |
Re: Home Sleep Lab < $1000
Jay, I have been following this thread since it started. It seems to me that just assembling some low costs diagnostic equipment would not give reliable results. Also, to interpret the complex data requires knowledgable professionals in the field.
In my case I would be happy to be able to rent some of the equipment, for once or twice a year {I don't need it for daily use} , that together with my own CPAP or APAP would provide most of the diagnosis that I could get from a full PSG at an OSA clinc. It could also verify the data I see daily in my CPAP.
Being on Medicare I am wondering if they (and other insurers) would pay for it if my Sleep MD prescribes it?
Here are a few possibilities of products and services:
http://www.sleepreviewmag.com/issues/pd ... ide_09.pdf
http://www.instantdiagnostic.com/ids/
Takes time to download the folowing:
http://www.instantdiagnostic.com/ids/do ... 0-2010.pdf
http://www.clevemed.com/clevemed_pdfs/M ... 20Intl.pdf
http://www.healthcare.philips.com/main/ ... efault.wpd
Any thoughts?
In my case I would be happy to be able to rent some of the equipment, for once or twice a year {I don't need it for daily use} , that together with my own CPAP or APAP would provide most of the diagnosis that I could get from a full PSG at an OSA clinc. It could also verify the data I see daily in my CPAP.
Being on Medicare I am wondering if they (and other insurers) would pay for it if my Sleep MD prescribes it?
Here are a few possibilities of products and services:
http://www.sleepreviewmag.com/issues/pd ... ide_09.pdf
http://www.instantdiagnostic.com/ids/
Takes time to download the folowing:
http://www.instantdiagnostic.com/ids/do ... 0-2010.pdf
http://www.clevemed.com/clevemed_pdfs/M ... 20Intl.pdf
http://www.healthcare.philips.com/main/ ... efault.wpd
Any thoughts?
_________________
| Mask: Mirage™ SoftGel Nasal CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: S9 Autoset machine; Ruby chinstrap under the mask straps; ResScan 5.6 |
Last edited by avi123 on Thu Oct 20, 2011 9:17 am, edited 1 time in total.
see my recent set-up and Statistics:
http://i.imgur.com/TewT8G9.png
see my recent ResScan treatment results:
http://i.imgur.com/3oia0EY.png
http://i.imgur.com/QEjvlVY.png
http://i.imgur.com/TewT8G9.png
see my recent ResScan treatment results:
http://i.imgur.com/3oia0EY.png
http://i.imgur.com/QEjvlVY.png
- Jay Aitchsee
- Posts: 2936
- Joined: Sun May 22, 2011 12:47 pm
- Location: Southwest Florida
Re: Home Sleep Lab < $1000
Hi Avi, I agree and disagree with what you've said. First, I think some low cost equipment as I have can provide some useful information. I also think those that have an S9 or equivalent, pulse oximeter and software as you do can tell as much about their sleep as they could with some of the "Home Study" equipment such as the IDS which is basically the same thing. If one didn't feel confident reading their results, they could always take them to their sleep doc for interpertaion. That said, some of the home study equipment, such as that from Cleveland, appears to have capabilities approaching a full blown PSG with multi channel eeg, etc. But now we're talking "big bucks".
I think medicare would pay for an in home study, but you'll have to find a Dr that has invested in the equipment. Most now it seems are investing in their own Sleep Labs and are raking in big money from it, so probably do not have the incentive to buy the home study equipment. You talk about "renting" the equipment, I don't have a clue about cost, but I'm sure you'd need a script and then a Dr to read it and I'm betting the cost of rental would be pushing at least $500, maybe more. Afterall, they getting something like $2000 for an overnight in their little sleep lab.
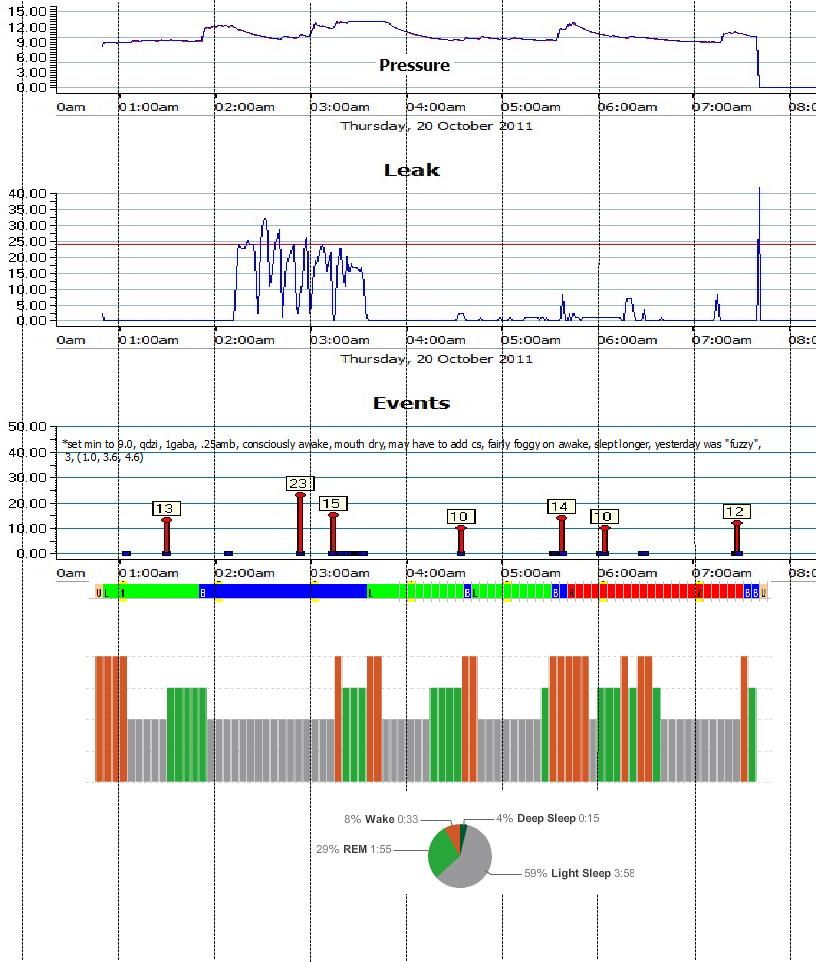
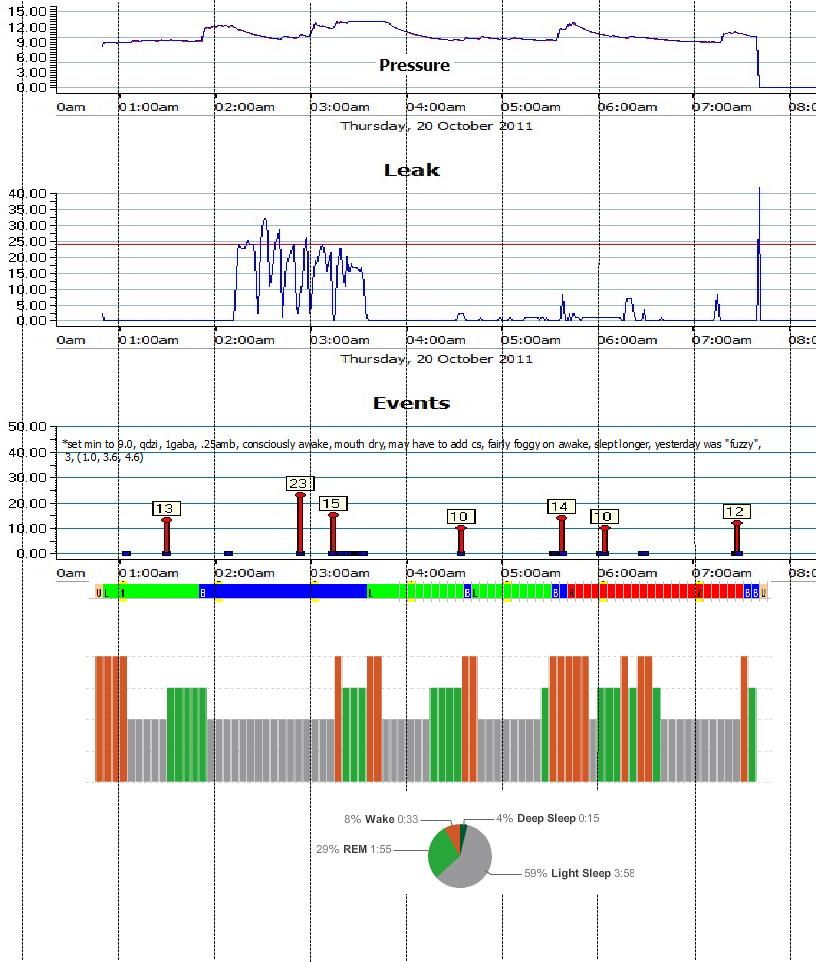
So, then there is my alternative. Indeed with shortcomings but cheap and comfortable. What I find to be the greatest shortcoming is the inability to monitor micro arousals. So I don't know if any one apnea or leg jerk actually disturbs by sleep. I don't know if alpha intrusions are causing my wakenings. I do know approximately: how many times I become fully awake, how much actual sleep, how much deep sleep, how much REM, how many apneas, how many destats (not shown on this chart) when these things occurred and what position I was in. Now, is any one night 100% accurate? No it's not, but over time the average accuracy will improve. Trends will develop and therein lies the value of my equipment. Over time I have objectice evidence if a therapy is working. If the amount of deep sleep is increasing, are awakenings decreasings, etc. Of course, the subjective "how I feel" measurement ultimately is most important, but it is a very unreliable indicator in the short run.
I see the equpment I put together as just a tool to help me evaluate my sleep. I certainly don't think it replaces a full blown PSG. It does help my doctor and me evaluate therapies.
I would very much like to get my hands on one of those Cleveland muti-channel devices but until I win the lotto, I'll have to settle for my Zeo.
Jay
Last Night's Summary
I think medicare would pay for an in home study, but you'll have to find a Dr that has invested in the equipment. Most now it seems are investing in their own Sleep Labs and are raking in big money from it, so probably do not have the incentive to buy the home study equipment. You talk about "renting" the equipment, I don't have a clue about cost, but I'm sure you'd need a script and then a Dr to read it and I'm betting the cost of rental would be pushing at least $500, maybe more. Afterall, they getting something like $2000 for an overnight in their little sleep lab.
So, then there is my alternative. Indeed with shortcomings but cheap and comfortable. What I find to be the greatest shortcoming is the inability to monitor micro arousals. So I don't know if any one apnea or leg jerk actually disturbs by sleep. I don't know if alpha intrusions are causing my wakenings. I do know approximately: how many times I become fully awake, how much actual sleep, how much deep sleep, how much REM, how many apneas, how many destats (not shown on this chart) when these things occurred and what position I was in. Now, is any one night 100% accurate? No it's not, but over time the average accuracy will improve. Trends will develop and therein lies the value of my equipment. Over time I have objectice evidence if a therapy is working. If the amount of deep sleep is increasing, are awakenings decreasings, etc. Of course, the subjective "how I feel" measurement ultimately is most important, but it is a very unreliable indicator in the short run.
I see the equpment I put together as just a tool to help me evaluate my sleep. I certainly don't think it replaces a full blown PSG. It does help my doctor and me evaluate therapies.
I would very much like to get my hands on one of those Cleveland muti-channel devices but until I win the lotto, I'll have to settle for my Zeo.
Jay
Last Night's Summary
_________________
| Mask: AirFit™ P10 Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: S9 Auto, P10 mask, P=7.0, EPR3, ResScan 5.3, SleepyHead V1.B2, Windows 10, ZEO, CMS50F, Infrared Video |
Re: Home Sleep Lab < $1000
Thanks Jay. In above posts you're talking about equipment that would replicate an almost full PSG clinic (except for doing Central Sleep Apnea Syndromes diagnisis with ASV machines for which you'll need an atendent for titration) for all sorts of OSA ailments. But in my case with plain OSA I have problems to find the effective pressure set-up on my S9 APAP for reducing the AHIs and also to make my sleep more " normal" by reducing the fragmentation, resolving the RES (Residual Excessive Sleepiness during the daytime), and improving my Epworth Sleepiness Score.
When I visited my Sleep MD last time, about a month ago, and while dicussining the above he asked me: "Will you be ready to pay for rental for those extra equipment? " and I could not answer on it not knowing the exact rental time and the financial arrangement. But I plan to find out. I suspect that this Doc who is part of a group of Internal Medicine Consultans which owns a Sleep Clinic whereby he is a part owner (a "sister" company), is talking about they buying the extra equipment and renting it to me. But let me find out if Medicare would pay for it.
Looking at your above graphs, I can presently, by using the ResScan, get all of them except the Zeo data and synchronising the Pluse Oximeter, timewise, with the ResScan graphs.
More to come.
When I visited my Sleep MD last time, about a month ago, and while dicussining the above he asked me: "Will you be ready to pay for rental for those extra equipment? " and I could not answer on it not knowing the exact rental time and the financial arrangement. But I plan to find out. I suspect that this Doc who is part of a group of Internal Medicine Consultans which owns a Sleep Clinic whereby he is a part owner (a "sister" company), is talking about they buying the extra equipment and renting it to me. But let me find out if Medicare would pay for it.
Looking at your above graphs, I can presently, by using the ResScan, get all of them except the Zeo data and synchronising the Pluse Oximeter, timewise, with the ResScan graphs.
More to come.
_________________
| Mask: Mirage™ SoftGel Nasal CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: S9 Autoset machine; Ruby chinstrap under the mask straps; ResScan 5.6 |
see my recent set-up and Statistics:
http://i.imgur.com/TewT8G9.png
see my recent ResScan treatment results:
http://i.imgur.com/3oia0EY.png
http://i.imgur.com/QEjvlVY.png
http://i.imgur.com/TewT8G9.png
see my recent ResScan treatment results:
http://i.imgur.com/3oia0EY.png
http://i.imgur.com/QEjvlVY.png
- Jay Aitchsee
- Posts: 2936
- Joined: Sun May 22, 2011 12:47 pm
- Location: Southwest Florida
Re: Home Sleep Lab < $1000
Avi, I've found the hardest part of my lab to "sync" is the pulse-oximeter, since it doesn't have real clock. What I do is try to create artifacts at known times, like put it on and take it off, so i can align it with the rest of the data. Fortunately, desats are not a major problem for me, so I don't wear it too often. I, too, suffer from fragmented sleep and lack of deep sleep. What I've been able to determine is that my sleep disturbances are not caused by REM - which is good since I understand that's the hardest to overcome. I'm also pretty sure my sleep is not being significantly interupted by apneas since my AI is usually down around 0.5 or less. That leaves pain and/or PLMD and my sleep Dr and I are are trying different meds to see if we can improve my sleep. I've just started on a new med and my apneas and awakenings are higher than normal which is not uncommon when I start a new therapy. So we'll give it a couple weeks and see how it develops. I am lucky to have found a Dr who encourages my participation in my own treatment. She treats the results of my "home sleep lab" with respect and we use them, in part, to determine the efficacy of treatment.
I'm not sure why you don't submit to a PSG to resolve some of the issues you are having. Is it because it's uncomfortable to go, or do you think the results would not be the same as at home? I don't know what medicare rules are, but I've had 3 in about 5 years. So, depending on your last, it's likely they would pay for another. It does sound as if something with a full EEG would be helpful in determining the cause of your fragmentation.
I would think you could get your AI under control with your S9 and ResScan. But, as I think you have said many times, that alone may not resolve all your sleep issues. I think many of us suffer from more than one type of sleep disturbance simultaneously and all we can do is tackle them one at a time. And that is precisely why I started to put together my own "lab".
Jay
I'm not sure why you don't submit to a PSG to resolve some of the issues you are having. Is it because it's uncomfortable to go, or do you think the results would not be the same as at home? I don't know what medicare rules are, but I've had 3 in about 5 years. So, depending on your last, it's likely they would pay for another. It does sound as if something with a full EEG would be helpful in determining the cause of your fragmentation.
I would think you could get your AI under control with your S9 and ResScan. But, as I think you have said many times, that alone may not resolve all your sleep issues. I think many of us suffer from more than one type of sleep disturbance simultaneously and all we can do is tackle them one at a time. And that is precisely why I started to put together my own "lab".
Jay
_________________
| Mask: AirFit™ P10 Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: S9 Auto, P10 mask, P=7.0, EPR3, ResScan 5.3, SleepyHead V1.B2, Windows 10, ZEO, CMS50F, Infrared Video |
-
davelikesbeer
- Posts: 250
- Joined: Tue Jun 21, 2011 11:45 pm
- Location: California
Re: Home Sleep Lab < $1000
Jay, you have inspired me. Actually, being on CPAP for four months, I'm sure my brain is starting to get back up to speed and that is helping as well. I was thinking of how to make a simple, yet inexpensive lab based on your work.Jay Aitchsee wrote:Avi, I've found the hardest part of my lab to "sync" is the pulse-oximeter, since it doesn't have real clock. What I do is try to create artifacts at known times, like put it on and take it off, so i can align it with the rest of the data. Fortunately, desats are not a major problem for me, so I don't wear it too often. I, too, suffer from fragmented sleep and lack of deep sleep. What I've been able to determine is that my sleep disturbances are not caused by REM - which is good since I understand that's the hardest to overcome. I'm also pretty sure my sleep is not being significantly interupted by apneas since my AI is usually down around 0.5 or less. That leaves pain and/or PLMD and my sleep Dr and I are are trying different meds to see if we can improve my sleep. I've just started on a new med and my apneas and awakenings are higher than normal which is not uncommon when I start a new therapy. So we'll give it a couple weeks and see how it develops. I am lucky to have found a Dr who encourages my participation in my own treatment. She treats the results of my "home sleep lab" with respect and we use them, in part, to determine the efficacy of treatment.
I'm not sure why you don't submit to a PSG to resolve some of the issues you are having. Is it because it's uncomfortable to go, or do you think the results would not be the same as at home? I don't know what medicare rules are, but I've had 3 in about 5 years. So, depending on your last, it's likely they would pay for another. It does sound as if something with a full EEG would be helpful in determining the cause of your fragmentation.
I would think you could get your AI under control with your S9 and ResScan. But, as I think you have said many times, that alone may not resolve all your sleep issues. I think many of us suffer from more than one type of sleep disturbance simultaneously and all we can do is tackle them one at a time. And that is precisely why I started to put together my own "lab".
Jay
One of the issues I was thinking of was the oximeter clock as well. It can be resolved if you connect it via USB to a computer. So the question is what computer would you use. I was just thinking this morning about using a router loaded with TomatoUSB may be possible. Basically, it's a cheap linux box. I recently bought an ASUS rt-n16 for about $75 because I wanted to connect my printer to it so it could be shared. It is a linux box, complete with wifi. In theory, you could connect a USB ir modified web cam to it for the full time or time lapsed video. You could also connect the oximeter to it.
The key is writing the software to support these devices. I believe jedimark is familiar with getting real-time data from the oximeters, so I know it is possible. I'm sure web cams can be done as well. It's just a matter of code (time).
Down the road, I think a usb bluetooth dongle would allow one to connect to the Zeo headband. I'm not sure what information the headband sends. I suspect it's the full on EEG data, then the receiver translates this into sleep levels.
I think such a setup could be very useful in tracking your own apena, but I think it could be used to help convince people thought to have apnea to see a doctor about it.
It would be cool if you could rig a CPAP to be in some kind of passive mode. For me, setting it to 4cmH20 would be just about the same as passive. But during a diagnostic study, they don't use a mask, and only have a sensor. It would be nice to have such a sensor as well. A quick search online find them at $120 and higher.
Dave.
_________________
| Mask: Swift™ LT Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: SleepyHead User. Tried liked Swift FX. Tried and didn't like Mirage SoftGel Nasal Mask. Previously used PSR1 Auto |
CPAP for the rest of your life.
Re: Home Sleep Lab < $1000
Jay Aitchsee wrote:Avi, I've found the hardest part of my lab to "sync" is the pulse-oximeter, since it doesn't have real clock. What I do is try to create artifacts at known times, like put it on and take it off, so i can align it with the rest of the data. Fortunately, desats are not a major problem for me, so I don't wear it too often. I, too, suffer from fragmented sleep and lack of deep sleep. What I've been able to determine is that my sleep disturbances are not caused by REM - which is good since I understand that's the hardest to overcome. I'm also pretty sure my sleep is not being significantly interupted by apneas since my AI is usually down around 0.5 or less. That leaves pain and/or PLMD and my sleep Dr and I are are trying different meds to see if we can improve my sleep. I've just started on a new med and my apneas and awakenings are higher than normal which is not uncommon when I start a new therapy. So we'll give it a couple weeks and see how it develops. I am lucky to have found a Dr who encourages my participation in my own treatment. She treats the results of my "home sleep lab" with respect and we use them, in part, to determine the efficacy of treatment.
I'm not sure why you don't submit to a PSG to resolve some of the issues you are having. Is it because it's uncomfortable to go, or do you think the results would not be the same as at home? I don't know what medicare rules are, but I've had 3 in about 5 years. So, depending on your last, it's likely they would pay for another. It does sound as if something with a full EEG would be helpful in determining the cause of your fragmentation.
I would think you could get your AI under control with your S9 and ResScan. But, as I think you have said many times, that alone may not resolve all your sleep issues. I think many of us suffer from more than one type of sleep disturbance simultaneously and all we can do is tackle them one at a time. And that is precisely why I started to put together my own "lab".
Jay
I'm not sure why you don't submit to a PSG to resolve some of the issues you are having ?.
reply to jay (only): Because I don't trust the technicians in the clinic that I used before. See here that about a year ago the effective titration result for me was for 6 cmH2O, however when I titrated my self to find out if I could get better results, see what happened:
There are better results at diff pressures:


So to carry out a new PSG I need to look for another place. But I do like my current sleep MD who partially owns this sleep clinic.
Also, if I could avoid doing PSG, often, why not find a In Home system which would indicate vital signs of wrong treatment and cost a lot cheaper?
p.s. Jay, looking at your graphs I don't see anything wrong and your events are miniscule. IMO, your sleep fragmentation comes from some underying medical conditions which are not related to respiration or sleep architecture. How about Diabetes, Depression, hi Epworth sleepiness score, alcohol, smoking, •Neurologic syndromes, etc.?
Or any of these causes:
This discussion includes the differentiation of various central sleep apnea syndromes from one another. Central sleep apnea in various forms can be seen in the following conditions or events:
•
Cheyne Stokes breathing-central sleep apnea: CSB-CSA is characterized by classic a crescendo-decrescendo pattern that typically occurs with a periodicity of 45 second or greater cycles (see image below). The ICSD-2[2] specifies that at least 10 central apneas and hypopneas per hour of sleep should occur, accompanied by arousals and derangement of sleep structure. The arousals occur at the peak of the hyperpnea phase. Patients usually have predisposing factors such as heart failure, stroke, or renal failure, as well as a lower resting PaCO2 than normal.
◦Heart failure
◦Stroke
◦Renal failureCheyne Stokes: This polysomnogram represents Cheyne Stokes breathing and occurred subsequent to continuous positive airway pressure titration for OSA in the same patient in the previous media file. Cheyne Stokes breathing has a classic crescendo-decrescendo breathing pattern.
•
Central sleep apnea due to a medical condition: The patient has a history of an underlying disorder other than heart failure or renal failure. Patients with stroke can have either classic CSB-CSA or central apneas without a crescendo-decrescendo pattern. ◦Stroke
◦Diabetes mellitus
◦Hypothyroidism
◦Parkinson disease
◦Multiple system atrophy or Shy-Dragger syndrome
◦Familial dysautonomia
◦Postpolio syndrome
◦Damage to medullary respiratory centers by tumor, infarction, or infection
◦Arnold-Chiari malformation types I-III
◦Cervical cordotomy
◦Muscular dystrophy
◦Myasthenia gravis
◦Prader-Willi syndrome
◦Idiopathic cardiomyopathy
◦Acromegaly
•
High-altitude periodic breathing: The single most important feature is that high-altitude periodic breathing occurs only with recent ascent to high altitudes. Many patients develop this at an altitude of 5000 meters or greater, while almost everyone develops it at an elevation of 7600 meters. The cycle length is shorter than in CSB-CSA, 12-34 seconds.
•
Use of opiates and other CNS depressants: This is most easily recognized by a history of opiate use. Wang et al[6] demonstrated that 30% of participants in a stable methadone maintenance program had a central apnea index (CAI) of greater than 5 and 20% had a CAI of greater than 10. Methadone blood concentration was significantly associated with the severity of central sleep apnea.
•
Primary central sleep apnea: This is an uncommon condition in which 5 or more central apneas, lasting 10 seconds or more, occur per hour of sleep. Patients have a low-normal PaCO2. The central apneas terminate abruptly with a large breath and without associated hypoxemia. They do not have a crescendo-decrescendo pattern of breathing
•
Complex sleep apnea: Central sleep apnea may emerge during titration of CPAP in patients previously diagnosed with obstructive sleep apnea. This syndrome, termed complex sleep apnea, has become a controversial topic in the sleep literature[17] and has been raised as a possible type of difficult-to-treat obstructive sleep apnea. As many as 6.5% of patients with obstructive sleep apnea may develop emergent or persistent central sleep apnea with CPAP treatment. CPAP emergent central sleep apnea is generally transitory and is eliminated after 8 weeks of CPAP therapy. Persistent CPAP-related central sleep apnea has been observed in approximately 1.5% of treated patients.[18] Similarly, complex sleep apnea can occur following a tracheostomy for obstructive sleep apnea. Central apneas have been found initially after a tracheostomy, but after an extended period, central sleep apnea decreased on repeat PSG.[19]
•
Physiologically normal apneic events ◦Central sleep apnea during sleep-wake transition: Up to 40% of healthy individuals may exhibit central apneas during sleep-wake transition. The central apneas occur during the period that chemoreceptors are resetting and instability of ventilation control occurs. They are usually brief and not associated with significant oxygen desaturation. The clinical significance of this entity is unknown. Once stable sleep is reached, normal individuals should not have more than 5 central apneas per hour of sleep.
◦Postarousal central apnea or postsigh central apnea: During a PSG review, central apneas are commonly seen following an arousal or after a sigh and are usually inconsequential. They are thought to be a result of Herring-Breuer reflex or hypocapnia induced by hyperventilation caused by a sigh or arousal.
Lets hope that there is none of the above.
_________________
| Mask: Mirage™ SoftGel Nasal CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: S9 Autoset machine; Ruby chinstrap under the mask straps; ResScan 5.6 |
see my recent set-up and Statistics:
http://i.imgur.com/TewT8G9.png
see my recent ResScan treatment results:
http://i.imgur.com/3oia0EY.png
http://i.imgur.com/QEjvlVY.png
http://i.imgur.com/TewT8G9.png
see my recent ResScan treatment results:
http://i.imgur.com/3oia0EY.png
http://i.imgur.com/QEjvlVY.png
- Jay Aitchsee
- Posts: 2936
- Joined: Sun May 22, 2011 12:47 pm
- Location: Southwest Florida
Re: Home Sleep Lab < $1000
Right on both counts! Ergo my home system and my ealier comments about having more the one problem. I feel I have the respiratory portion under control, althought it took me a number of years to do it. And I think you hit the nail on the head about not trusting the techs. It's not that they're incompetent. I think it's because they're working with only one data set. A person goes to the lab, gets titrated (which may be right for that night under those conditions) and is sent home with a CPAP and a pressure setting. I think a person is extremely lucky if that works for them. For me it didn't work, I didn't feel better, so I wasn't compliant. It took a couple years for me to learn I could get data from my CPAP. Once I did, I started self titrating and got my AHI down to around 6 or so. I found the software, bought an autoset out of pocket, became compliant and got my AHI down to around 3. I have learned an APAP works better for me, that my ideal pressures changes with time, and that even though I have the respiratory portion under control I still don't get restorative sleep. Now, I was diagnosed with moderate to severe apnea and severe PLMD so I knew I had more than one problem, but I feel earlier attempts to treat the PLMD failed because I was not compliant and the only measure of success was whether or not I felt better. Well, of course I didn't feel better, I wasn't compliant so the PLMD meds might have worked but my sleep was fragmented by the apnea so there was no way to know. Now my Dr and I are trying the meds again and just last week we ordered full blood work to help rule out the things you mentioned. This included a metabolic panel, kidney function, Vitamins D, B's, iron, thyroid, etc., I am waiting the results now. I am hopeful that I will eventually find the root cause of my non-restorative sleep (I didn't see statins in your list) or at least a med that will treat it, but I don't expect it to be easy.avi123 wrote:.... Also, if I could avoid doing PSG, often, why not find a In Home system which would indicate vital signs of wrong treatment and cost a lot cheaper?....
p.s. Jay, looking at your graphs I don't see anything wrong and your events are miniscule. IMO, your sleep fragmentation comes from some underying medical conditions which are not related to respiration or sleep architecture. How about Diabetes, Depression, hi Epworth sleepiness score, alcohol, smoking, •Neurologic syndromes, etc.?....
So, back to you, I'm not sure I understand your data, but it looks like your best pressure is around 7? Don't you have an autoset now? When I was doing my titration with a CPAP, the best advice I got from a sleep Dr was to start low. My prescibed pressure was 10 and I was working around that but not getting anywhere. One problem was leaks. I couldn't get them under control. So I went to 7 and stayed there untill I got the leaks under control. Then I increased my pressure by .5 and stayed there until I got my leaks under control or at least a week. I found it took some time for my AHI to stabilize after a change in pressure. I kept this up until I reached about 9.5, my AHI had dipped and I started back down. Anyway, I ended up about 8.5. When I got my autoset, I set it for 7-12 and its median pressure came back at about the same around 8.4, but because it could control some of the apneas that needed a higher pressure, my AHI dropped. So, my point is I think self titration is possible, but it's a slow process even with an APAP. It appears to me the body must be given time to adjust after each change and leaks must be controlled or titration won't be successful.
Avi, this is a long rambling post the point of which I'm not sure, but I think we agree about treatment; some type of self monitoring is probably necessary for success, sleep disturbances aren't necessarily limited to respiratory factors, and those that expect to feel better just because they get a cpap are likely to be dissapointed - it takes work.
_________________
| Mask: AirFit™ P10 Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: S9 Auto, P10 mask, P=7.0, EPR3, ResScan 5.3, SleepyHead V1.B2, Windows 10, ZEO, CMS50F, Infrared Video |
- Jay Aitchsee
- Posts: 2936
- Joined: Sun May 22, 2011 12:47 pm
- Location: Southwest Florida
Re: Home Sleep Lab < $1000
Dave, I'm going to leave the code writing to you younger guys. The last code I wrote was FourTran IV or maybe some early BASIC
I use a laptop now to run my webcam for the video and I could do the oximeter with usb at the same time, I just haven't spent the time to get it working. It's another wire and since desats haven't been a problem, I just haven't been motivated.
I'm waiting for you guys to build a little box to sync everything, should be easy enough, just a little beyond my current capabilities. In the meantime, my system is a little crude but it works for me. Especially since the Zeo's first line graphic is to the nearest 5 minutes. (to the nearest 30 sec is available and tallied in reports)
Let me know when you've got the box
jay
I use a laptop now to run my webcam for the video and I could do the oximeter with usb at the same time, I just haven't spent the time to get it working. It's another wire and since desats haven't been a problem, I just haven't been motivated.
I'm waiting for you guys to build a little box to sync everything, should be easy enough, just a little beyond my current capabilities. In the meantime, my system is a little crude but it works for me. Especially since the Zeo's first line graphic is to the nearest 5 minutes. (to the nearest 30 sec is available and tallied in reports)
Let me know when you've got the box
jay
_________________
| Mask: AirFit™ P10 Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: S9 Auto, P10 mask, P=7.0, EPR3, ResScan 5.3, SleepyHead V1.B2, Windows 10, ZEO, CMS50F, Infrared Video |